Month: December 2019
-
Controlling Beta Cell Proliferation and Apoptosis to Manage Type 1 Diabetes
A key indicator of type 1 diabetes is lack of insulin-producing beta cells in the pancreas. These cells are mistakenly attacked and destroyed by the immune system leaving individuals unable […]
-

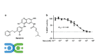
Leveraging the Power of Light to Manage Type 1 Diabetes
A common problem in managing type 1 diabetes is maintaining relatively stable blood glucose levels. By the time a person realizes their blood sugar is rising or falling and begins […]
-

Improving Vascularization of Transplanted Islet Cells
One option that researchers have explored for treating type 1 diabetes is cell transplantation. By introducing new pancreatic islet cells, they aim to better control glucose levels and insulin production. […]
-

Expanding Type 1 Diabetes Research Through Marmoset Models
It is not uncommon for researchers to use animal models for initial research before transitioning to human clinical trials. Many animals’ systems are biologically similar in nature to humans and […]
-

Exploring the Use of Targeted Proteins in Managing Type 1 Diabetes
Currently, the most effective treatment for type 1 diabetes is the administration of insulin, but this is not a perfect solution. Since the body is unable to produce enough – […]
