Final Project Update
It is well known that the mTORC1/4E-BP2 axis has beneficial effects on beta cells, and control Treg cell number and function. Based on that, the main goal of this project was to investigate how the mTORC1/4E-BP2 axis is involved in the prevention of type 1 diabetes (T1D). With that purpose, we deleted one protein of the mTORC1 pathway in the non-obese diabetic (NOD) mouse background, a mouse model that develops type 1 diabetes spontaneously and similarly to the human disease. In this one year, we investigated: (i) glucose homeostasis, islet morphology and function before, during and after diabetes onset; (ii) islet function under stress conditions; (iii) lymphocyte population in the pancreas and peripheric tissues and (iv) the capacity of lymphocytes to induce T1D. Since these knock-out mice are protected from type one diabetes development, the results obtained during the program allowed us to better understand the role of mTORC1 in two major components in the pathogenesis of T1D: autoimmune response and beta cell survival, making us excited about the possibility of developing new therapies for type 1 diabetes in the future.
6-Month Project Update
It is well known that the mTORC1/4E-BP2 axis has beneficial effects on beta cells and
control T reg cell number and function. Based on that, the main goal of this project is to investigate how the mTORC1/4E-BP2 axis is involved in the prevention of type 1 diabetes (T1D). With that purpose, we deleted one protein of the mTORC1 pathway in the non-obese diabetic (NOD) mouse background, a mouse model that develops type 1 diabetes spontaneously and similarly to the human disease. In these first 6 months, we investigated the islet morphology and function before, during, and after diabetes onset. We also evaluated the lymphocyte population in the pancreas and peripheric tissues. The results allow us to better understand the role of mTORC1 in two major components in the pathogenesis of T1D: autoimmune response and beta cell survival, making us excited about the possibility of developing new therapies for type 1 diabetes in the future.
Project Description
Type 1 diabetes (T1D) is an autoimmune disease in which the immune system destroys insulin-producing cells (beta cells) in the pancreas, reducing insulin levels and leading to high blood glucose. Regulatory T (Treg) cells are immune cells that help the body recognize itself; they prevent autoimmune diseases, including T1D.
mTORC1 is a protein complex that functions as a nutrient sensor and controls protein synthesis. mTORC1 regulates Treg cell development, number and function. In addition, mTORC1 activation of one of its targets (4E-BP2) increases the number of beta cells. More importantly, beta cells lacking 4E-BP2 are resistant to treatment with cytokines – immune proteins that can cause cell death. However, the extent to which 4E-BP2 deletion prevents type 1 diabetes development in mice is unclear.
Since the mTORC1/4E-BP2 pathway has beneficial effects on beta cells and helps control Treg cell number and function, we hypothesize that it could be involved in T1D prevention by increasing beta-cell survival and regulating autoimmunity. This project could lead to novel T1D therapies targeting the two major components in the development of T1D: autoimmune response and beta-cell survival.
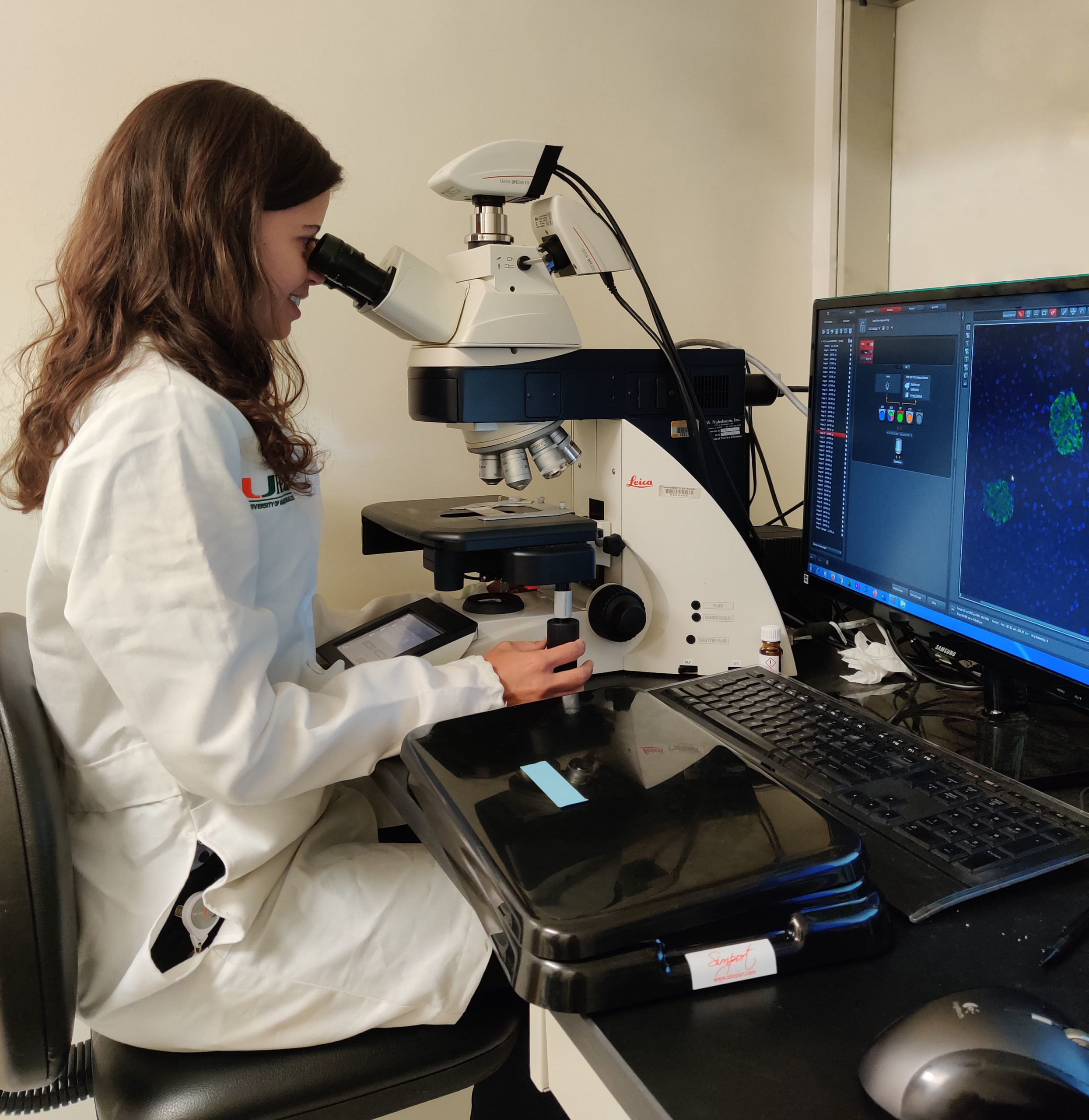
To assess this hypothesis, we have assembled a multidisciplinary research group composed of researchers with expertise in beta cell biology, intracellular signaling, diabetes, and immunology.