Where is She Now?
Wendy Yang, Ph.D. had the results of her DRC-funded project published at Connexin 43 Functions as a Positive Regulator of Stem Cell Differentiation into Definitive Endoderm and Pancreatic Progenitors. DRC staff recently connected with her and she wanted us to pass on her gratitude to our supporters: “I appreciate this community so much! The process of pulling together the video for the website helped launch my path into biotech commercialization.”
Final Project Report
Wendy Yang successfully completed this project supported by DRC and in doing so she earned her PhD degree in the Department of Pharmacology at the University of Washington (Seattle). The project focused on an innovative strategy to increase the homogeneity of stem cell-derived Definitive Endoderm cells, that in turn mature more efficiently into pancreatic islet progenitors. In the study, Dr. Yang was able to manipulate the function of a special class of proteins called Connexins which are responsible for connecting cells during their growth and development into different cell types. The results of these studies are currently under review for publication.
Read Other Project Updates Here
Project Description
My project centers on finding new ways of generating insulin producing cells from human stem cells. I focus on understanding basic mechanisms of cell to cell communication in stem cells during their development into immature pancreatic cells, and eventually insulin-producing cells.
Type 1 diabetes (T1D) is also referred to as juvenile onset diabetes. It is a devastating disease affecting more than 1 million people in the U.S. and is typically diagnosed during childhood. There are 15,000 children diagnosed with the diseased annually and they must learn to tightly regulate and control this disease for the rest of their lives.
T1D patients no longer produce their own insulin, a hormone made in the pancreas that is responsible for maintaining steady levels of blood sugar. In an unaffected person, eating a donut will cause the body to release insulin, which acts as a key to let sugar enter cells in the body where it can be used to produce energy. In a person with T1D, there is no insulin to let sugar enter the body’s cells. Consequently, all of the sugar remains in the bloodstream unable to be used. This high blood sugar can result in a number of short and long term complications including blindness, heart disease, and organ failure, especially in the kidneys. Currently, the only viable option for T1D patients to survive is to take multiple daily injections of insulin to keep their blood sugar levels under strict control.
My research focuses on the development of new cell replacement strategies to restore insulin production in patients with T1D. Specifically, my goal is to turn stem cells into new insulin-producing cells that can one day be used for transplant. This process is already defined but I seek to increase the quantity of pancreatic cells we can generate.
To do this, my experiments aim at understanding and modifying the function of a class of proteins called Connexins which are responsible for connecting cells during their growth and development into different cell types in the body. These proteins function by forming small channels across cells that stick to one another. Think of adjacent cells as rooms in a house, Connexins act as a door between them to let things in and out. These channels are used by stem cells to exchange biochemical information and make collective decisions to either grow and expand, or acquire specific characteristics such as becoming a cell of the brain, heart, skin, or pancreas. These channels act as very selective gates of cell communication that are used by cells to exchange a variety of messages.
In line with this notion, I recently discovered that stem cells treated with a chemical to increase the function of Connexins exhibit a much higher propensity to become insulin-producers compared to untreated stem cells. It appears that promoting cell-to-cell communication during growth of immature pancreatic cells leads to increased numbers of insulin-producing cells. There is a technical bottleneck in generating large numbers of cells that can produce significant levels of insulin. In perspective, although a lab may be able to produce a couple million insulin-producing cells, we would need billions for a viable transplant. My discovery is important because it shows a connection between Connexin function and the ability to derive insulin producing cells.
This discovery of Connexin function relative to stem cell maturation may have a significant impact on the development of innovative new strategies to derive the cells we need for future use in transplantation for T1D patients. I am incredibly excited about where these experiments will lead and I am seeking you help in funding the studies. I am confident we can find the way to cell-replacement therapies for T1D.
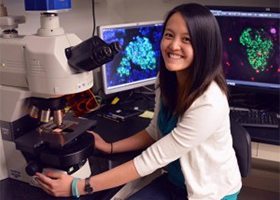
About Me
Hello, my name is Wendy Yang. I a a Ph.D. candidate at the University of Washington. I am from Farmington Hills, Michigan about 25 miles outside of Detroit. I have always believed in patient-tailored medicine as the future of the field and science as the driver of that innovation. Choosing diabetes research was a way to pioneer studies at the intersection of science and medicine. It provided an outlet for me to participate in cutting edge research that I hope will actively improve diabetes therapies in the near future.