Where is he now?
Yo Suzuki, Ph.D. of J. Craig Venter Institute, and his team received follow on funding to continue his important work. He recently reported, ” We are making progress with the project. The main challenge is to make a sufficient amount of insulin in our skin bacterial platform to have an effect on the body. We are testing multiple strategies. Please stay tuned for updates in this exciting research,” Yo Suzuki, Ph.D. of J. Craig Venter Institute.
Final Project Update
The generous grant from the DRC enabled the critical first step toward a microbial treatment for diabetes that circumvents the struggle of injected insulin therapy. We reached a milestone to demonstrate deep-skin bacteria producing and secreting insulin. Moreover, the knowledge we gained and the materials we generated with the DRC support will strengthen our next efforts, which are now clearly defined because we experienced aspects of the work already. Securing funding for the subsequent work was also an important goal. Regarding this, we are happy to report that our skin bacteria work is part of a project headed by our team member John Glass to be funded by the Larry L. Hillblom Foundation. Therefore, our future efforts will become a reality.
Read Other Project Updates Here
Project Description
Success will bring more NIH funding and could eliminate needles!
Insulin delivery using infusion pumps can be effective for treatment of T1D, but it does not completely protect T1D patients from the long-term effects of the disease or enable a normal non-diabetic lifestyle. Diabetes research has focused on using insulin-producing cells isolated from cadavers or made from stem cells in T1D patients. While some of the research has yielded promising results, nothing yet has radically changed general approaches to treat patients.
Our approach is to give bacterial cells that naturally live in our body the ability to function like our insulin-producing cells, to synthesize insulin when blood glucose levels are high to maintain proper glucose levels in T1D patients. In the proposed project, we will establish the feasibility and safety of this approach by making bacterial strains with this function and testing them in mouse systems. If successful, our research will form the basis for a bacterial treatment that can circumvent the struggle of injected insulin therapy and the issues regarding the rejection of transplanted human cells.
Project Details
An important ingredient of our study is a set of bacteria recently discovered to naturally reside deep within the human skin, in a layer previously thought to have only human cells. This layer of the skin contains blood vessels and is, therefore, suitable for implanted cells to monitor blood glucose levels and release insulin for systemic distribution. These bacteria do not cause problems in our body. Unlike transplants, they do not trigger host immune response. Unlike insulin pumps, they can enter this deep layer of the skin without puncturing the skin!
Advances in biology now enable making changes to DNA, the genetic material, in these bacteria. Our team at the J. Craig Venter Institute is at the forefront of these advances to produce safe and beneficial bacteria. To make the deep-skin bacteria function like insulin cells, we will introduce a gene into them for making a version of insulin. Bacteria cannot make native insulin by themselves, but there is a type that can be made in bacteria and is as effective as native insulin. We will also introduce a DNA piece containing three genes for making a glucose sensor to control insulin production in the bacteria.
It is critical that insulin-producing bacteria do not infect healthy individuals. Therefore, we will install a mechanism to prevent the bacterial cells from spreading beyond the designated host. We will then paint the mouse skin with our bacteria and see if blood glucose levels drop.
This critical proof-of-concept experiment will tell us if this skin bacteria-based approach has promise and deserves continued support. If we are successful, we will have experimental data that will attract additional funding from the NIH. Establishing a system that can be tested in actual T1D patients will involve many rounds of experimentation and improvement. For example, our future bacterial cells will have more sophisticated safety features. However, tools needed for this approach are already available in basic form. Moreover, the eventual product may be superior to any other products under development. Therefore, we strongly feel that the work needs to be started now toward determining the viability of this approach. Your support could help revolutionize T1D therapy.
Needles be Gone for T1D Slideshare
About Me
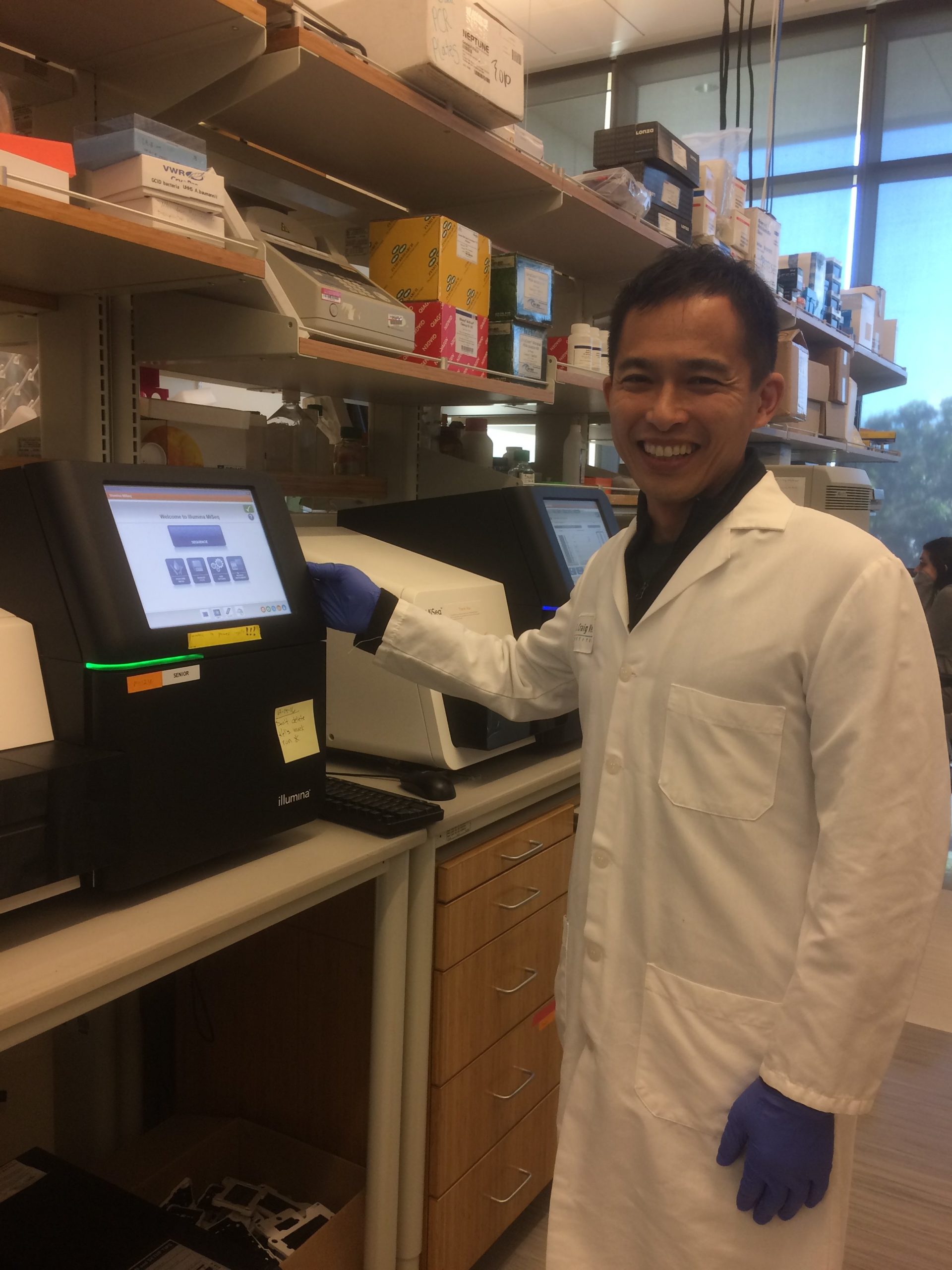
Hello, my name is Yo Suzuki. I am an Assistant Professor at the J. Craig Venter Institute. Our institute is known for its expertise in reading and writing genomes, blueprints for life. When writing genomes, our focus is to design and build beneficial microbes. I have been engineering microbes for 11 years, and finally, a connection is made between my skills and the opportunity to contribute to curing type I diabetes. The goal of this project is to create a bacterial strain that can respond to glucose and produce potent insulin analogs in a mouse. Our long-term goal will be to develop an engineered bacterial strain as a surrogate for beta cells in T1D patients. If we are successful, we will have a microbial treatment that circumvents the struggle of injected insulin therapy and problems with a transplant approach. Our project is the first and critical step toward this long-term goal. Our approach is innovative, but many tools to enable this approach are already available, including harmless bacteria that enter the skin in a non-invasive manner and live in a layer of skin appropriate for glucose sensing and insulin administration. Our tools to control these bacteria will only improve. Therefore, we have to start the work now to test the viability of this promising approach. Your support is greatly needed and appreciated.