Month: June 2019
-

Is it Possible to Delay the Onset of Type 1 Diabetes?
Living with type 1 diabetes (T1D) is challenging. It requires constant monitoring and adjustment of one’s blood sugar. Since T1D is commonly diagnosed in childhood, it can put additional strain […]
-

Scientists Uncover New Insight into Autoimmune Response
Autoimmune diseases are challenging to treat because the immune system plays a critical role in keeping the body healthy. However, when this system is destroying its own cells even without […]
-

Exploring Protective Factors Against Diabetic Kidney Disease
One of the complications that can stem from living with diabetes is the risk of developing diabetic kidney disease. The kidneys play a critical role in filtering waste and excess […]
-

Connect For A Cure: May 2019 Newsletter
Welcome to the May edition of the Diabetes Research Connection newsletter! We aim to keep you updated with our latest achievements, upcoming events, and how you can get involved in […]
-
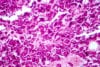
Beta Cell Proliferation May Help Protect Against Type 1 Diabetes
In individuals with type 1 diabetes (T1D), the body’s immune system mistakenly attacks and destroys insulin-producing beta cells. For years, researchers have been looking at options for suppressing this immune […]
