Month: February 2015
-
Early Signs in Young Children Predict Type 1 Diabetes
New research shows that it is possible to predict the development of type 1 diabetes. By measuring the presence of autoantibodies…
-
Protein That Repels Immune Cells Protects Transplanted Pancreatic Islets From Rejection
Transplanting islets encapsulated with CXCL12 restores blood sugar control without immunosuppression in animal models of diabetes…
-
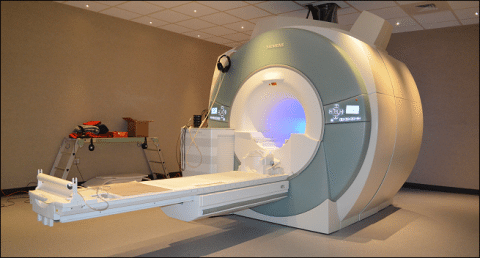
Scientists Use MRI to Visualize Pancreas Inflammation in Type 1 Diabetes
A pilot study led by researchers at Joslin Diabetes Center has revealed that it is possible to use magnetic resonance imaging (MRI)…
-

FDA Approves Lucentis for Treatment of Diabetic Retinopathy in People With Diabetic Macular Edema
Genentech, a member of the Roche Group, has announced that the U.S. Food and Drug Administration (FDA) approved…
-

‘Smart’ Insulin May Ease Burden of Type 1 Diabetes Patients, Research Suggests
Diabetes patients could be spared the burden of constantly monitoring blood sugar levels after scientists have developed…
-

Change in Gut Bacteria May Precede Type 1 Diabetes in Kids
THURSDAY, Feb. 5, 2015 (HealthDay News) — In some young children who develop type 1 diabetes, a change in normal stomach…
-

Stanford Researchers Discover Insulin-Decreasing Hormone in Flies, Humans
An insulin-regulating hormone that, until now, only had been postulated to exist has been identified by researchers…
-

A Simple Method to Monitor β Cell Death in Individuals At-Risk for Type 1 Diabetes
Type 1 diabetes is characterized by death and reduced function of β cells, which produce insulin. The presence of specific…
-

Inhaled Insulin Powder Now Available in Pharmacies
PARIS and VALENCIA, Calif. — Afrezza, an inhaled insulin powder, is now available by prescription in U.S. retail pharmacies, Sanofi…
