Speeding Up Insulin Activation for Managing Type 1 Diabetes
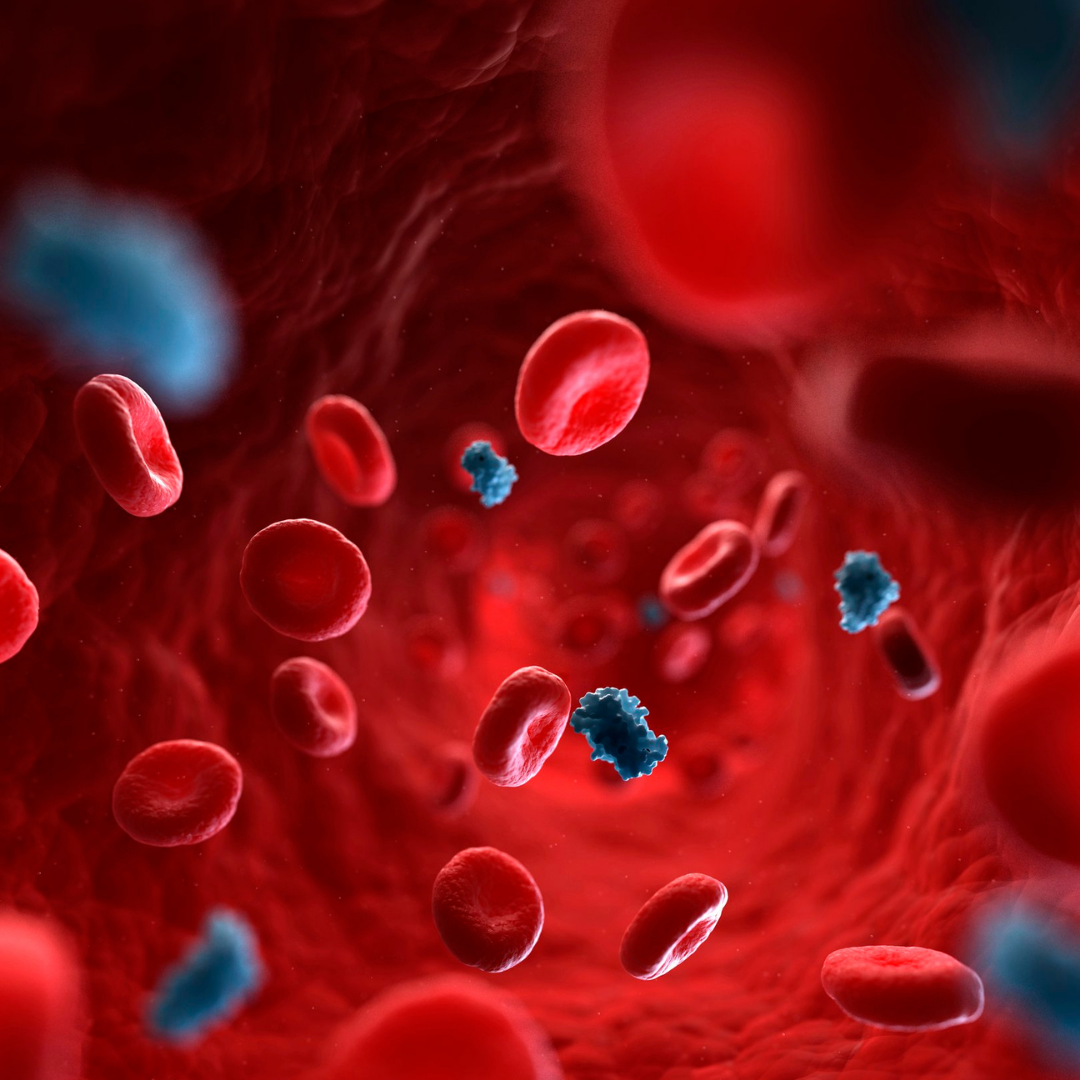
Individuals with type 1 diabetes (T1D) rely on daily insulin injections to effectively manage blood sugar levels and maintain glycemic control. Because blood sugar rises when eating, fast-acting (or rapid-acting) insulin is typically administered just before mealtimes to help curb this spike and begin lowering blood sugar more quickly.
Fast-acting insulin generally begins working within about 15 minutes, peaks within about 90 minutes, and lasts about four hours total. Of course, each person responds differently, and the effects can vary based on numerous factors including the amount of carbohydrates eaten, blood glucose level before eating, injection site, activity, and more.
Researchers have been searching for a way to expedite this process by activating insulin more quickly. Traditional insulin contains a combination of monomers, dimers, and hexamers, with monomers acting the fastest and hexamers taking the longest to break down. A recent study found that using monomeric insulin alone can start decreasing blood glucose levels almost immediately.
The biggest challenge is that these monomers are very unstable and are attracted to the top of the liquid in the vial. Once they hit the air, they aggregate within two hours and become inactive. By using a special polymer blend, scientists were able to create a barrier at the liquid’s surface and keep the monomeric insulin more stable, lasting for more than 24 hours under stress. Commercial insulin only remains stable for about 10 hours. With the addition of the polymer, even commercial insulin increased its duration of stability for up to a month.
The effectiveness of this ultrafast insulin was tested on diabetic pigs, and results showed that the “insulin reached 90 percent of its peak activity within five minutes after the insulin injection. For comparison, the commercial fast-acting insulin began showing significant activity only after 10 minutes. Furthermore, the monomeric insulin activity peaked at about 10 minutes while the commercial insulin required 25 minutes.”
Researchers are planning to apply for approval to test this ultrafast monomeric insulin in human clinical trials, but no trials are planned as of yet. The speed at which this insulin formulation activates as well as the increased stability could improve blood sugar management options for individuals with type 1 diabetes. In addition, this type of insulin could be beneficial in advancing artificial pancreas devices.
Although more testing is needed, this ultrafast insulin could be a game-changer for some individuals with type 1 diabetes if it performs safely and effectively in human trials. Diabetes Research Connection (DRC) is excited to see how these findings continue to unfold and what it could mean for the future of diabetes management.
Though not involved with this study, the DRC plays an active role in supporting research around T1D by providing up to $50K in funding to early-career scientists pursuing novel, peer-reviewed research. To learn more about current projects and how to help, visit http://localhost/drc.