Original article written by Bradley J. Fikes and published by The San Diego Union-Tribune on April 15, 2016. Click here to read the original article.
Salk Institute scientists say they’ve discovered a key ingredient needed to make functional insulin-producing beta cells. With that knowledge, the scientists say they can realize a dream in treating Type 1 diabetes: growing replacement beta cells from the patients themselves.
If these replacement cells can be implanted and protected, they will make insulin as the body needs, just as the original cells do. That means type 1 diabetes would, for the first time ever, be curable.
The ingredient is a protein called ERR-gamma that turns up energy production in the beta cells, said Ron Evans, a Salk researcher who co-led the study with colleague Michael Downes. These cells are made from artificial embryonic stem cells, called induced pluripotent stem cells. Typically produced from skin, these IPS cells cells are being examined for their potential to treat a variety of diseases.
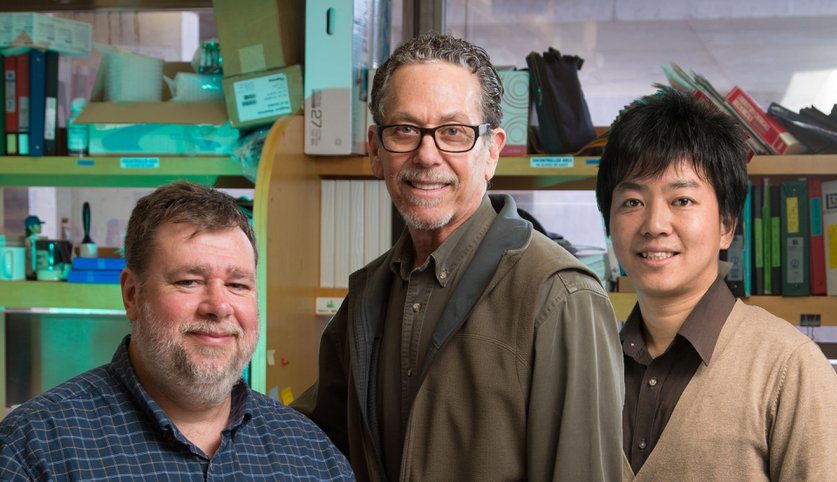
The study, published Tuesday in the journal Cell Metabolism, provides more evidence that cell replacement therapy may eventually provide a cure for type 1 diabetes, caused by the destruction of beta cells through an autoimmune reaction. The study can be found atj.mp/evansbeta. The first author was Eiji Yoshihara, first author of the paper and a Salk research associate.
Type 2 diabetes is even more common than Type 1. In the United States as of 2012, about 1.25 million children and adults have type 1 diabetes, and 29.1 million had the type 2 form, according to the American Diabetes Association. In San Diego County as of 2012, about 140,600 or 6.2 percent have type 2 diabetes.
In type 2 diabetes, the body becomes resistant to insulin, and the pancreas may become disease and have trouble producing sufficient insulin. As a result, blood sugar rises beyond normal, producing all sorts of damage. This can include weight gain, heart problems, poor limb circulation leading to amputation, kidney disease and blindness. These patients may also come to require insulin.
Disease reversal
Unlike the first kind, type 2 diabetes can be reversed, at least in some cases. Dieting and exercise leading to weight loss is key, according to recent research. A 2013 study in the journal Diabetes Care found that causing patients to burn more substantially more calories than they consume, either by diet or bariatric surgery, restores insulin sensitivity over a period of 8 weeks.
Bariatric surgery, which a portion of the gut is removed to limit food absorption, appears to reverse type 2 diabetes in nearly all patients, according to other studies.
But diets are notoriously hard to adhere to, and bariatric surgery is a drastic step many people are reluctant to take. So scientists are focusing on how type 2 diabetes arises in the first place, with the hope of finding some way of preventing it from taking place at all.
A 2014 study by UCSD researchers led by Dr. Jerrold Olefsky found that a lack of oxygen in fat cells is the trigger that starts the process that ends up causing type 2 diabetes. The study, published in the journal Cell, examined the disease in mouse models, considered a good proxy for human diabetes.
It reported that certain fatty acids, especially saturated fats, increased the need for oxygen in fat cells, causing them to fall into an oxygen-deprived state. This led to inflammation, an immune reaction and insulin resistance.
If the study results are borne out in people, it may be possible to produce a drug that would stop this process in the bud. It won’t stop obesity, but the most drastic health problems would be prevented.
For type 1 diabetes, no treatment exists to reverse the disease.
A very limited form of cell replacement therapy is already used for those with the most dangerous form of type 1 diabetes. They get transplants of islet cells or pancreases from cadavers. Those treated belong to a small subset of type 1 diabetics who get no warning signs that their blood sugar has fallen too far. They can die as a result.
Cell replacement
San Diego’s ViaCyte is already testing a replacement therapy using progenitor cells derived from human embryonic stem cells. In animal testing, these cells mature into beta and other pancreatic “islet” cells.
Another approach with induced pluripotent stem cells is being researched in the lab of Harvard University researcher Douglas Melton. He and colleagues have come up with their own formula for producing beta cells, and published studies outlining the approach.
Melton’s group reports that the cells express genetic activity very similar to adult beta cells, and regulated blood sugar when transplanted into mice whose own beta cells were destroyed.
These therapies all face difficulties, the trickiest perhaps being the patient’s own immune system, which destroyed their own islet cells in the first place.
Islet and pancreatic transplant patients are given immunosuppresive drugs. These drugs are toxic and make the patients more vulnerable to infection. Therefore, these procedures are used only on type 1 diabetics at greatest risk, said Julia L. Greenstein, vice president of discovery research at the research foundation JDRF.
ViaCyte has pioneered another approach to the problem. The islet cells are encapsulated in a semipermeable membrane that keeps out the immune system, but allows nutrients to flow in, and insulin and waste products to flow out. Moreover, the islet cells may potentially produce other blood sugar-relating hormones besides insulin.
Whether that strategy works is the point of clinical testing of ViaCyte’s product, now in a Phase 1 trial. This trial tests for safety. Participants receive easily removable implants of encapsulated cells, which are expected to mature in place and produce insulin. These implants are being removed periodically and examined to make sure the maturation process is going smoothly and that the membrane remains intact.
Presumably, other stem cell-based replacement therapies such as that the Salk scientists or Melton are developing will require an immune system-blocking barrer like ViaCyte’s, to protect the cells. Meanwhile, research continues on ways to modulate the immune system of type 1 diabetes to stop the autoimmune reaction.
Power to the cells
The Salk Institute’s Evans said applying the ERR-gamma protein promotes the growth of mitochondria, the power plants of cells. This gives the cells energy to make insulin.
“It turns on the light, it turns on the energy that flows into the cell. And that we think is the missing link,” Evans said. “It is a switch that controls mitochondrial numbers and activity. You really rev up the power of the cell. Instead of having a weak or indolent cell, you rev it up to the level that it needs to be able to release insulin in response to glucose. And that takes a lot of energy.”
In mouse models, the effect of the therapy is immediate, he said.
“The day that we implant them, the diabetes starts going away,” Evans said. “These cells, you can purify them in a dish. You can grow them exactly the way you want, to hundreds of millions of cells that all share common features. For human therapy, you need that.”
Further research may enable production of different islet cells that make other important hormones to regulate blood sugar, Evans said. And a few more years of testing and preclinical development, it should be possible to test the therapy in humans.