Imagine popping a pill covered in tiny steel needles – that you cannot in any way feel – to quickly and effectively lower your blood glucose.
Or swallowing a glucose-lowering capsule that’s only activated when you shine a blue LED light on your stomach.
We are not making this stuff up. Even though the concepts sound like top tags for the proverbial Diabetes Wall of Weird, they are both actually real-life drugs currently under development and being tested in research here in the U.S. and abroad.
A Pill Covered with Needles?
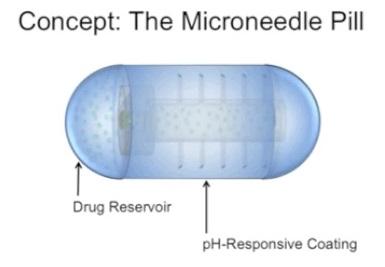
First, the Microneedle Pill is being developed by a team of researchers at the Massachusetts Institute of Technology (MIT) and Massachusetts General Hospital who recently published their work in the Journal of Pharmaceutical Sciences.
They’ve created an acrylic capsule 2 centimeters long and 1 centimeter in diameter, that includes a reservoir for the insulin and is covered with hollow, stainless steel needles about 5 millimeters long. But don’t be too afraid — there’s a dissolvable coating covering the needles so they won’t be exposed while moving down into your system.

Here’s how it would work:
- You’d swallow the pill and let it travel on down your throat into the GI tract, made safe by the protective coating and apparently that part of the body doesn’t have any pain receptors, so you wouldn’t feel a thing.
- Once inside your GI tract, the pH-sensitive coating on the pill would dissolve and the small microneedles would be uncovered, to inject insulin into the lining of the stomach, small intestine, and colon.
- Researchers are working to make this method even safer by using needles made of degradable polymers and sugar that would break off, embed in the GI tract and continue delivering insulin as the sugar molecules disintegrate. Wait, insulin and sugar… isn’t that the D-version of creating a pill that combines fire and water?
As noted in the video, researchers have tested this first-gen microneedle pill on a handful of pigs, and the results showed the insulin was successfully delivered without any signs of tissue damage. And yes, the pigs’ blood glucose levels decreased more quickly from this insulin delivery method than when they were given traditional insulin injections.
Aside from treating diabetes, the researchers believe this method could be used for any treatment that now requires injections — making it potentially “revolutionary.”
This research has gotten a good amount of media attention in the past few weeks; we couldn’t help rolling our eyes at the way MIT’s own press release preempted the inevitable sensational media headlines by clamoring: “New drug-delivery capsule may replace injections.”
Yes, we’d prefer to do away with shots, but the idea of swallowing needles (no matter how small) still seems a little scary, no? Especially when you see the images, like this one courtesy of the MIT press folks:
Ugh… that pill looks pretty Halloween from where I sit. What if the protective coating over the needles dissolves too quickly and it snags in someone’s throat? Or what if one of those little needles breaks off too early and gets caught somewhere… else?
Can’t help mulling over that point.
‘Just Flick the Lightswitch’ Pill?
The second new drug from the Weird Wall is an oral agent aimed at type 2 PWDs (people with diabetes) that only works when you shine a light on your stomach. So nothing scary, but definitely a little out there…
In a study published on Oct. 14 in Nature Communications, a group of international researchers explain their prototype known as JB253, a “photoswitchable sulfonylurea” that would kick-start insulin release from the T2 pancreatic cells when exposed to blue light. The authors are Dr. David Hodson and Professor Guy Rutter at Imperial College London, and Professor Dirk Trauner and Dr. Johannes Broichhagen at LMU Munich.
It’s a capsule that looks just like any other pill you would take with a meal and let dive deep down into your stomach. And in your body, it actually works to lower glucose in the same way as existing sulfonylureas drugs, widely used to treat T2 diabetes. Except that this one doesn’t do anything at first. Not until you shine a blue LED light on your abdomen (that may be adhered to your skin using adhesive, like a small non-invasive sensor), activating the pill and changing its shape inside you to turn on the glucose-lowering capability. And the light activation would be reversible, so you could easily switch off the light and stop the medication from doing its thing.
Wait, like a Kmart blue light?? Well, it’s actually violet-blue, the form of light needed to penetrate the skin, and only a very small amount of light is needed to activate the drug, researchers say.
As explained in this in-depth article in the Diabetes News Journal, the big advantage over existing sulfonylureas is that this new, light-activated delivery method would lower the risk of these meds causing hypoglycemia and even cardiovascular risk,.
Just like the microneedle-pill scientists, these researchers believe they may be on to the Next Big Thing in Medicine — light-activated meds that could lead to a safer, more controllable version of therapy for a number of illnesses.
“The idea is that light-sensitive drugs could be administered in the form of a pill, then released or activated by irradiating a patch of skin with a blue LED. When the light is switched off the drug flips back into the inactive form… Light can be controlled with exquisite precision, which allows us to target the receptor of interest with very high specificity. In addition, the activating reaction is itself reversible,” researcher Dr. Trauner explains.
Sounds weirdly intriguing, but of course there’s nothing to do but wait and see. “We have a long way to go before it will be possible to use such a therapy in patients,” researcher Dr. Hodson admits.
OK, maybe one thing we CAN do is appreciate these seemingly Mad Scientists who are willing to go out on limb for the sake of a promising idea. Seriously, today’s CGMs would have probably seemed just as “out there” to the PWDs of yesteryear…