Big Picture
· On June 28, the FDA approved Lantidra, which is the first cellular therapy to treat type one diabetes. (FDA Press release)
· 21 out of 30 participants who received Lantidra treatment did not need to take insulin for at least a year, including 10 participants who did not need to take insulin for more than five years.
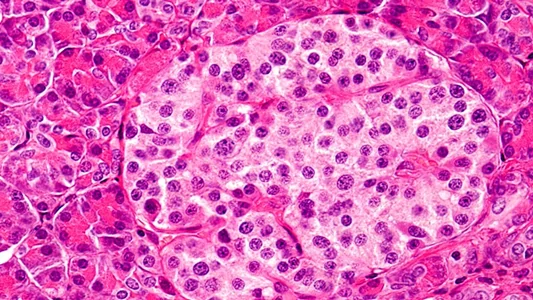
How does this cellular therapy work?
Pancreatic cells from a deceased donor are transplanted into a patient with T1D to replace insulin-producing beta cells, which help control blood glucose (BG) levels. Lantidra is the first commercialized therapy. It builds on decades of experimental islet cell transplants.
Who is eligible to receive Lantidra?
Patients with T1D need daily insulin therapy. Some develop hypoglycemic unawareness, which may lead to sudden and severe low BG levels, which may result in a coma, seizures, or death. The FDA approved Latidra treatment only for adults with T1D and hypoglycemic unawareness.
How well does Lantidra work?
Lantidra therapy was tested in two non-randomized studies. Each T1D participant with hypoglycemic unawareness received 1-3 infusions of Lantidra. The goal was for participants to become insulin independent, eliminating the need for daily insulin injections and self-regulation of BG without patient intervention. Five participants never became insulin-independent, 21 were insulin independent for a year or more, 11 were insulin independent for 1-5 years, and 10 were insulin independent for over 5 years.
Does Lantidra have side effects?
One major drawback of this therapy is the need for immunosuppression drugs to prevent rejection of the transplanted islets. The intensity of these side effects related to the number of infusions received. The number and severity of side effects varied and included nausea, diarrhea, fatigue, anemia, and abdominal pain. Some severe complications required stopping the use of immunosuppressants, which caused the death of the transplanted cells and loss of insulin independence. A majority of participants reported at least one serious negative effect from the combined Lantidra and immunosuppressant therapy.
How will this FDA approval impact type 1 diabetes therapy?
Since Latidra is approved only for T1Ds with hypoglycemic unawareness and is likely to be expensive, this therapy will help a small percentage of those with T1D to achieve insulin independence. Continuous glucose monitoring and automated insulin devices may also alleviate the hypoglycemic unawareness issue but is not a cure.
Where do we go from here?
Considerably more research is needed to develop a safe, cost-effective T1D cure without immunosuppression. Vetted, novel approaches are supported by DRC donors. Cures may include artificial beta cells, immune-privileged islet cells generated from stem cells, smart insulin and other potential therapies to universally treat individuals living with T1D. DRC continues to monitor advancements and fund innovative approaches to end T1D.
Vincenzo Cirulli and Alberto Hayek, the current and past Chairs of DRC’s Scientific Review Committee, comment on FDA approval of Lantidra:
Lantidra’s cadaveric islet transplant technology was first published in 2000 during the Edmonton trials. It has not progressed much since then, other than some improvement in drugs used to address the rejection of transplanted islet tissue. The rapidly evolving progress witnessed over the past few years with stem cell-derived islet cells, currently being used in pilot clinical studies, indicate that stem cell-derived islets will likely supplant cadaveric islets transplants very soon. Unlike cadaveric islets, an exciting advantage of stem cell-derived islet cells is that they are amenable to genetic and epigenetic modification to allow their engraftment without the need for immunosuppression, and possibly prevent the recurrence of autoimmunity. This, although at an early stage, is an avenue of translational research that is likely to lead to a permanent cure for T1D. In the meantime, T1D researchers must be adequately supplied with high quality cadaveric islets for their research, as they will continue to provide a gold-standard quality control to monitor and compare the functional maturity of stem cell-derived islet tissue.
How will competition for this very limited resource be allocated, and at what cost? DRC will continue to support peer-reviewed, innovative, and unbiased solid science to finally put an end to T1D.