CGM Use In Hospitals
Covid-19 patients who have diabetes experience a higher mortality rate than the general population. A new protocol incorporates the use of continuous glucose monitors (CGM) to track and manage hospital patients’ blood glucose (BG) levels before problems arise. Monitoring and treating glucose levels is critical for patients with diabetes.
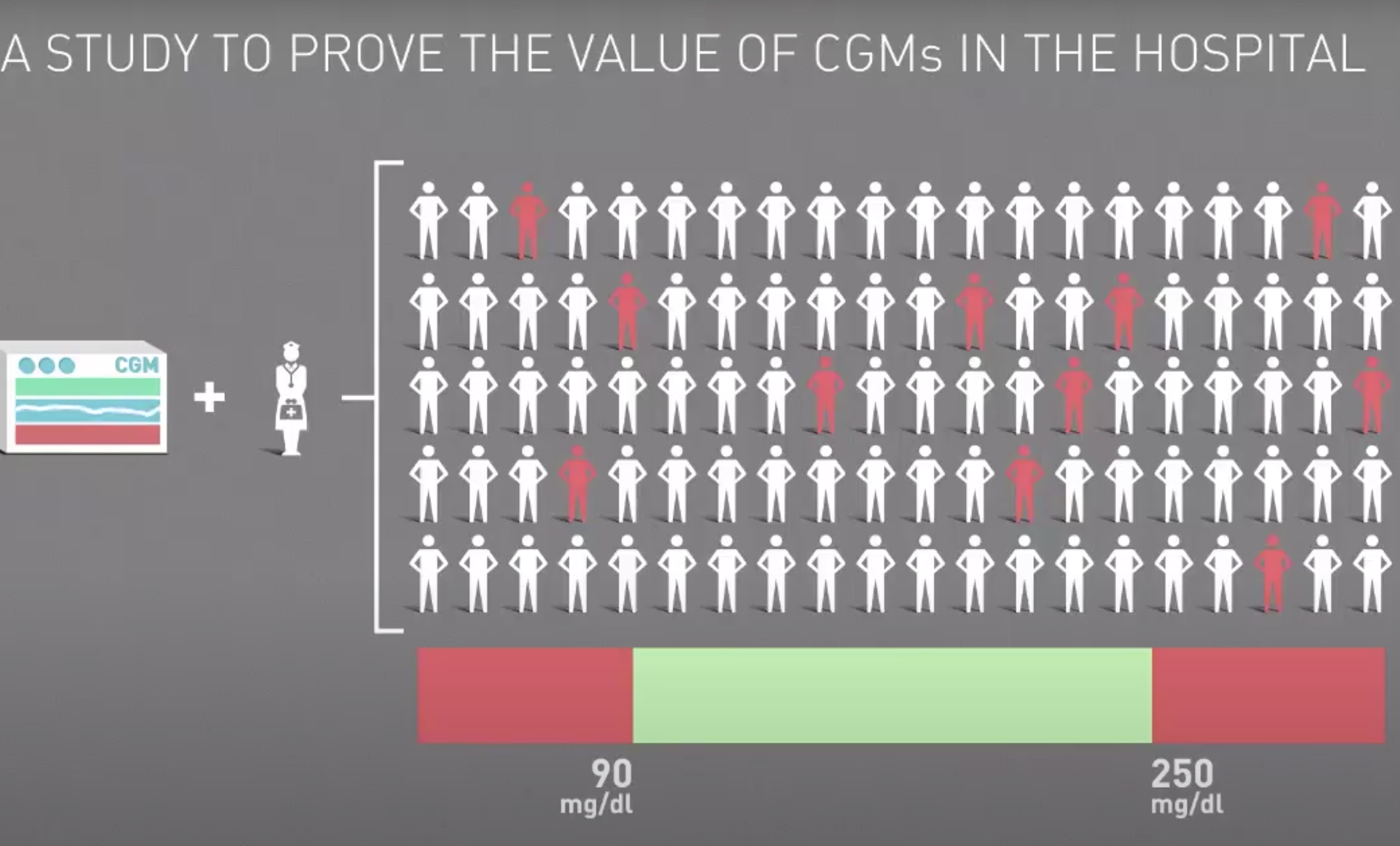
A clinical study conducted by Scripps Whittier Diabetes Institute (SWDI), Glucose as the Fifth Vital Sign: A Randomized Controlled Trial of Continuous Glucose Monitoring in a Non-ICU Setting, was led by the Scripps Whittier Diabetes Institute’s (SWDI) Addie Fortmann, Ph.D. with support from the Diabetes Research Connection (DRC). The use of CGM in hospitals has the potential to enhance care, reduce the length of stays, and yield improved outcomes, as well as greater patient satisfaction. “The current pandemic environment has greatly accelerated the need to find safe and effective ways to monitor the blood sugar of hospitalized patients without interfering with the necessary and often intensive interventions to treat COVID-19,” said Addie Fortmann, Ph.D., director of the diabetes service line at Scripps and the lead author of the paper. “Our study clearly demonstrates the value of CGM in community hospitals, and it offers a model for other health systems that are looking to use this technology in similar ways.”
“DRC’s funding helped to enable Scripps to evaluate effects of CGM in a hospital in a study setting and use the experience to expedite deployment of this important glucose monitoring system when the FDA provided emergency use authorization (EUA) in March of this year,” according to Dr. Alberto Hayek, Scientific Advisor at SWDI, endocrinologist, former T1D researcher at SWDI and UCSD, and President and co-founder of DRC. When individuals are hospitalized, diabetes management is more difficult. Not only are patients dealing with the condition which brought them to the hospital, their blood sugar levels must be continuously monitored, which is very difficult if the patient is on a ventilator or is unconscious.
The U.K. National Health Service (NHS) recently published research concluded hospitalized individuals with type 1 diabetes (T1D) are significantly more likely to die from COVID-19 than those with type 2 diabetes (T2D). Preliminary findings, recently published in Diabetes Care, determined a third of people with T1D and COVID-19 in the U.S. experienced diabetic ketoacidosis, from elevated BG, and half experienced hypoglycemia (low BG). Both of these serious conditions can lead to death. Individuals with T1D typically do not produce insulin which presents serious challenges to managing inpatient BG.
“Tracking vital signs is routine in many hospitalized patients,” said Athena Philis-Tsimikas, M.D., corporate vice president of Scripps Whittier and the senior author of the report. “This study demonstrates that blood sugar should be considered the fifth vital sign for hospitalized diabetes patients, joining temperature, pulse, respiration and blood pressure, as a potentially crucial metric for delivering the highest quality care.”
A CGM uses a small sensor that is inserted under the skin. It sends a glucose reading via Bluetooth every five minutes to hospital staff so that they can track glucose levels and receive alerts when levels start to rise or fall out of the target range.
David Winkler, co-founder of DRC, Chair of the Board, has been living with this autoimmune disease for more than 60 years. He has experienced several challenging hospital stays himself and said, “I strongly endorse Scripps’ exciting new CGM protocol to lessen the serious concerns T1Ds experience in the hospital environment. I applaud Scripps for this material paradigm shift.”
The DRC is excited to see how this clinical research will influence hospital protocols nationally to provide enhanced care for patients with diabetes by better managing their blood glucose levels during a hospital stay.
Dr. Hayek added, “Our non-profit funds novel T1D research nationally. DRC’s 80 member Scientific Review Committee peer-reviews all grants, including this breakthrough clinical trial.”
To learn more about the T1D research projects supported by DRC and how this charity provides hope for treatment and cure of this disease, please visit http://localhost/drc.