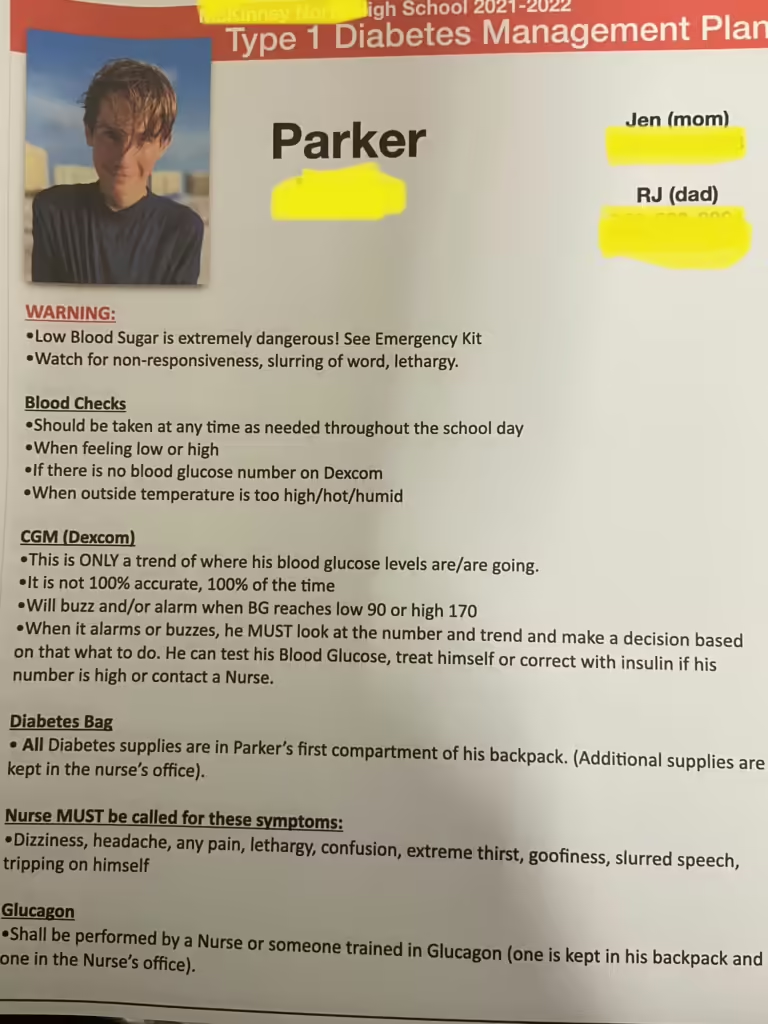
As the back-to-school season nears, parents of children with Type 1 diabetes (T1D) face unique challenges. Preparing your child to manage T1D at school requires careful planning and communication. In this post, T1D mom Jen Poston shares her advice. Her son Parker was diagnosed at 6 (now 18 and just graduated high school), and her daughter Madison was diagnosed at 4 (now 15 and starting her sophomore year). From creating diabetes management plans to fostering independence, Jen’s tips will help ensure a smooth, stress-free school year for your child, whether they are starting kindergarten or high school.
Don’t miss our companion blog, “Back to School with T1D,” addressing the emotional and social challenges and offering practical solutions for a supportive environment. Together, these resources will equip you with the knowledge and tools to support your child’s journey through the school year.
Practical Tips from a T1D Mom
Hearing from parents who have firsthand experience managing their child’s T1D in a school setting is invaluable. In this Q&A, Jen shares how she has successfully navigated the ups and downs of managing T1D for her two children throughout their school years. Her insights and strategies can help you and your child tackle the upcoming school year. Here are some of Jen’s top tips that have made a real difference in her family’s journey with T1D.


How do you prepare your child for the school day to ensure they manage their blood sugar levels effectively?
We discuss their schedule for the day, including any physical activities or tests, which might impact their blood sugar. We make sure they know how to handle any potential issues that might arise. This preparation helps them feel confident and ready to manage their diabetes independently. Additionally, we have a routine for checking blood sugar levels before school and make sure their diabetes devices are working properly and have sufficient battery charge or supplies.
What essential items do you pack in your child’s diabetes care kit for school?
In my child’s diabetes care kit that they carry on them, I include:
- A blood glucose meter, test strips, and lancets for checking blood sugar levels.
- Insulin in their pump, along with alcohol swabs for sanitizing injection sites.
- Snacks such as juice boxes, granola bars, or candies for treating low blood sugar.
- A glucagon emergency kit in case of severe hypoglycemia. (GVOKE/Baqsimi) There is one carried on them at all times, and another at the nurse’s office.


In the nurses’ office:
- Spare batteries/chargers for devices and insulin pumps (this is kept at the nurse’s office in their box).
- Extra infusion sets and insulin reservoirs.
- Extra Dexcom sensorsKetone strips to test for ketones in case of high blood sugar (we use Blood ketone strips-NOT urine ketone strips as that checks ketones from the past).
- Bottles of water, juice boxes, and snacks.
- Fresh insulin in their fridge.


How do you educate and inform your child’s teachers and classmates about T1D?
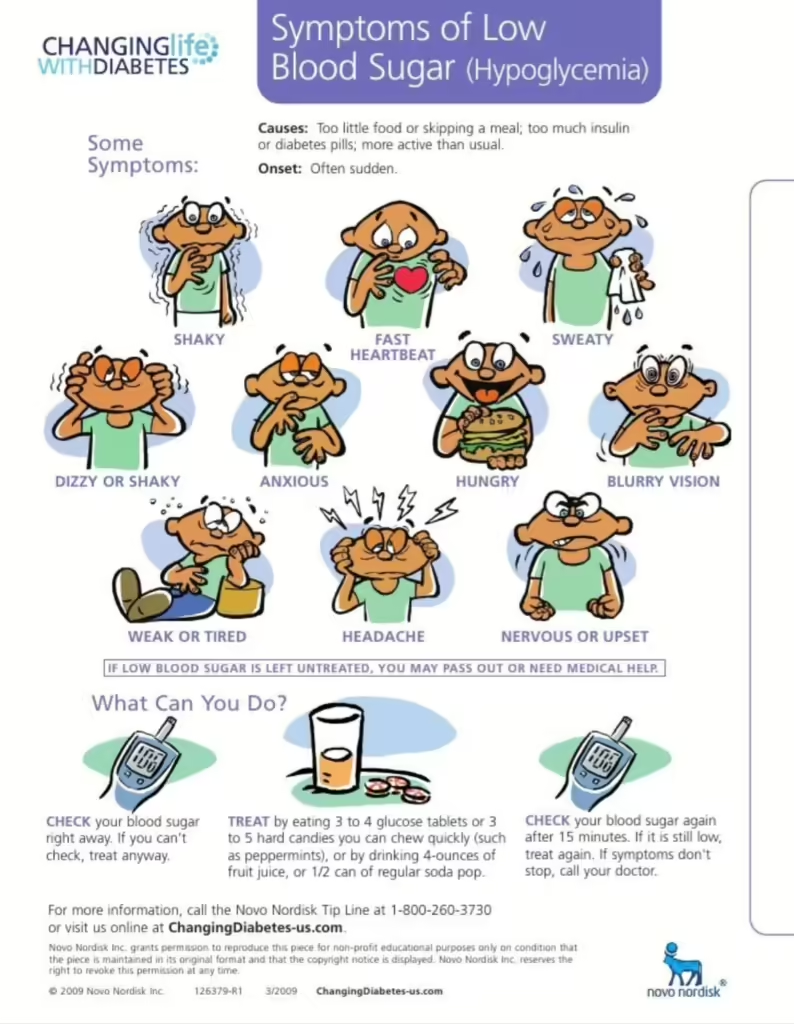
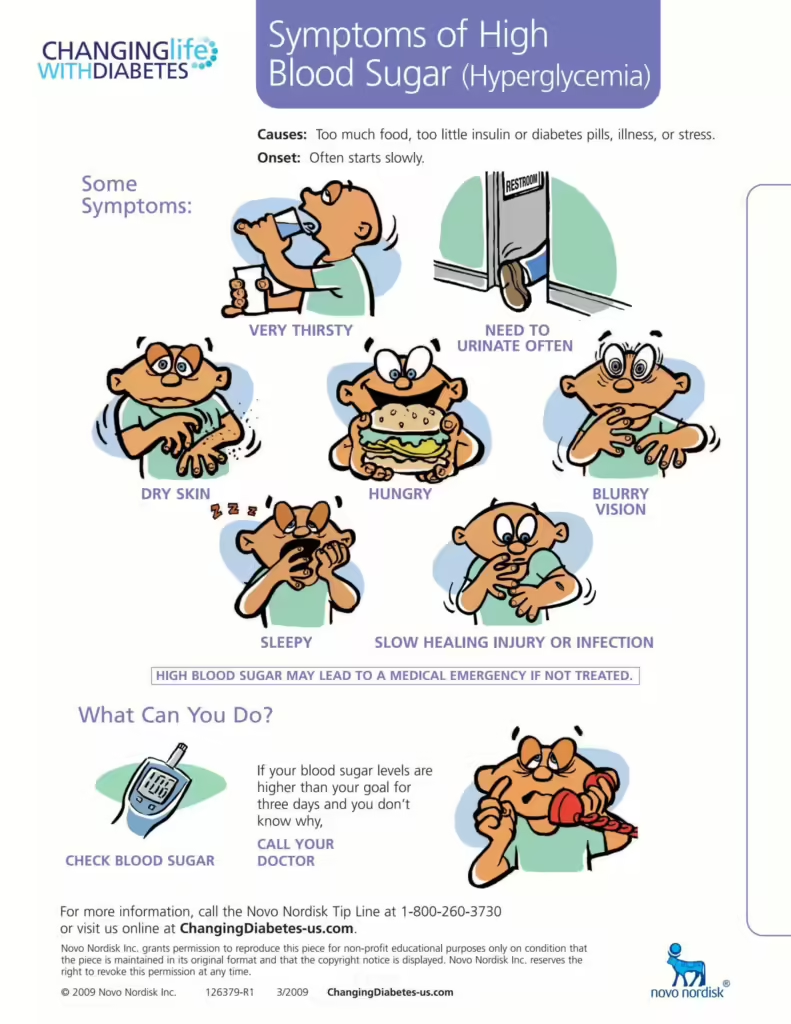
At the beginning of the school year, I schedule a meeting with my child’s teachers, the school nurse, and other relevant staff to explain what T1D is, how it affects my child, and what signs to look out for in case of high or low blood sugar. I provide a detailed written plan that includes emergency procedures, contact information, and specific instructions for handling diabetes-related issues. For classmates – when they were little I would visit the class to give a brief, age-appropriate presentation about T1D. I’d bring in an age-appropriate book to read and some diabetes supplies to show them. This helps avoid any stigma of T1D and encourages a supportive environment. Starting from preschool and now at high school level, I have always prepared red binders for each and every teacher. Within these red binders is a personal info sheet of my child on the first page. Then in individual sheet protectors are pages of facts, hypoglycemia, hyperglycemia, language etiquette, Dexcom CGM information, etc.

What strategies have you found most effective for handling blood sugar fluctuations during school hours?
Regular monitoring and communication with the school nurse are crucial. Our children wear a continuous glucose monitor (CGM) that provides real-time updates on their blood sugar levels, alerting both my child and me to any significant changes. We have established a protocol for checking blood sugar at specific times, such as before meals, after physical activity, and whenever they feel symptoms. I ensure my child understands how to adjust their insulin, based on their readings and activities. Having quick access to snacks and drinks helps manage sudden blood sugar drops. We also review their day each evening to discuss what worked and what might need adjusting. When they were younger (pre-K to about 3rd grade) we solely communicated with the nurse (usually by phone) to discuss what to do for a plan of action (ex., pre-carbing for lunch). As they matured, we moved to texting them and having them answer us on their Apple watch.
How do you ensure your child has access to necessary snacks and insulin throughout the school day?
I coordinate with the school to make sure my child can access their diabetes supplies and snacks at any time. We keep a supply of non-perishable snacks in their classrooms (art, PE, music, etc) and the school nurse’s office. I also provide my child with a small, portable kit that contains quick-acting sugar sources and necessary diabetes supplies. I work with the school to allow my child to carry their insulin and testing kit in their backpack /fanny pack (depending on their age at all times).
Our children have always done insulin pump therapy (except for the first 11 months after Parker’s diagnosis). So they always had “access” to insulin. However, it wasn’t until they were “labeled” independent on their 504 and health plan that they were able to dose the insulin themselves. They were able to go to the nurse at any time they needed for a correction if their sugars were too high.
For snack time or lunchtime, it was more important to me that they went to lunch with their peers and sat with them. To make this work successfully, we had them leave the classroom (always with a buddy) five minutes before snack or lunchtime to see the nurse to go over carbs and administer insulin. By the time they were dosed/corrected, they’d meet their class in the halls and were able to join them for snack/lunch.
What advice do you have for setting up and maintaining a 504 plan or other accommodations with the school?
Oh my, SO much advice and help. First and foremost, our children do not attend school at all until the 504 is in place, and all teachers have been trained. Therefore, we hold our 504 meetings before school is in session…usually about 2-3 days before school starts. I still prefer in-person, however, zoom meetings can work as well. I think the most important points are:
- Always, always have an emergency plan.
- Decide where supplies are kept at all times (testing supplies, low blood-sugar supplies, water, and then, of course, who has GVOKE or Baqisimi (emergency treatment that can be administered for severe low blood sugar).
- Plan if the school goes on lockdown. Having a lockdown protocol in place ensures that your child will have access to any supplies needed during a lockdown. Supplies should always be on the child.
- What about recess, lunch, and PE? We found in the early years of preschool and elementary, we used a red fanny pack with a medical alert patch sewn on it. Inside was a juice box, GVOKE, and a testing kit. Either the PE teacher or the yard duty staff would be handed this by my child to hold while my child did PE and/or recess/lunch. My child was responsible for always getting it back when recess/lunch/PE was over and it was brought back to class. We had a safe place where it hung by the classroom door. So, it was there to grab easily as they exited class and then easily returned as they entered.
- ALL tardies and absences related to T1D were/are NOT held against them or counted against them. THIS is a big deal, especially as they age into high school. If Madison had a late night due to high blood sugars and felt yucky in the morning, with exhaustion; we’d let her sleep a bit and then take her in late. But that tardy was excused since it was related to T1D. The same with lows during the night. Sometimes, it’s as simple as you’re rushing out the door, and they announce, “Oh mom, my pump is almost out of insulin!”, so then we’re tardy for making sure their pancreas was fueled!
- School Testing/Exams. Ugh… this was a tough one and one that has changed over the years. For standardized testing: iPhones were in range for them so we could see blood sugars via Dexcom; They had access to water the entire time and a snack, if needed; If at any time a test is “paused” due to either a high or low blood sugar, our child can make up that time.
- Be thorough when documenting all necessary accommodations, such as the ability to check blood sugar, administer insulin, access to snacks, bathroom breaks, and the ability to participate fully in all activities. Ensure the plan includes provisions for handling emergencies and substitute teachers. Maintain open communication with the school staff and document all meetings and correspondence.
How do you prepare your child for emergencies, and what protocols have you established with the school staff?
UGH-the topic that no one wants to discuss – emergencies! There are a few different types of emergencies: lockdowns, fire drills, low bg (blood glucose), high bg with blood ketones (we use a blood ketone meter, NOT the urine ketone strips as they are testing ketones from a while ago, not present), and the fear of all fears – a severe hypoglycemia episode.
We practice emergency scenarios at home, so my child knows exactly what to do if they experience severe high or low blood sugar. I provide the school with a detailed emergency action plan that includes symptoms of hyperglycemia and hypoglycemia, treatment steps, and emergency contact information. Several staff members, including teachers and the school nurse, are trained on how to recognize symptoms and administer glucagon (GVOKE) if necessary. We also have a clear protocol for contacting me or another emergency contact if my child needs immediate medical attention.
It is also imperative that our kids know what to do during a lockdown. Each of our children’s teachers has a plastic bin in their classroom filled with water, juice, a snack, and a low treat. However, what if your kiddo is outside the classroom – perhaps walking down the hall, and a lockdown siren goes off and they are pulled into a different room? What good is the “bin” that is in your child’s classroom? That is why it is important that ALL supplies are always on them.
We have experienced three hypoglycemia events resulting in three seizures and 911 calls. Unfortunately, every event was different and handled differently. Overall, the school handled it correctly, but there were still some lessons we all walked away with.

What methods do you use to foster your child’s independence in managing their T1D while at school?
I encourage my child to take an active role in their diabetes management by teaching them to recognize symptoms, check their blood sugar, and administer insulin. We set small, achievable goals to build their confidence and independence, such as learning to calculate carbohydrate intake or understanding how different activities affect their blood sugar. Regularly reviewing their day and discussing what worked or what challenges they faced helps reinforce their learning. Open communication is key, so I make sure they feel comfortable asking for help when needed and praising their efforts and successes to build their self-esteem. Being able to text them via their watch is imperative to us. Over the years, we slowly gave them more responsibility over time. It could be as simple as filling their supplies in their bags each day. The most important thing is to watch for diabetes burnout.
How do you address your child’s emotional well-being and mental health with their diabetes management?
Oh, THIS is a tough one and ONE that is not spoken of enough. Managing a chronic condition like T1D IS stressful, so I make it a point to talk openly about their feelings and experiences. I encourage them to express any frustrations or fears and reassure them that it’s normal to feel this way sometimes. We connect with support groups and other families managing T1D to provide a sense of community and understanding. I also ensure they have access to a counselor or therapist if needed, to help them cope with any emotional or mental health challenges that arise. We have used these resources in the past multiple times. Diabetes burnout is a REAL thing.
What tips can you share for maintaining open and effective communication with your child’s teachers and school staff regarding their diabetes care?
Collaborating with the nurse and teacher is key. As a parent, you want them to follow your health plan and 504. You are your child’s best advocate. YOU are your child’s voice. However, it’s sometimes a fine line. You need to collaborate and everyone needs to have your child’s best interest in all decisions. Establishing a good relationship/rapport with the school staff from the beginning is crucial. Using a communication notebook or a digital app can help keep everyone informed and ensure that messages are shared promptly. We chose texts and emails, as they are documented. I encourage teachers and staff to ask questions and express any concerns they might have at any time. In a growing youth, T1D is constantly changing. What works in September may no longer work by December. Being approachable and responsive when the school has questions or concerns is important.
These practical tips from Jen can make a significant impact on how you and your child handle the school year with T1D. Remember, you’re not alone in this journey. By sharing knowledge and supporting one another, we can create a better environment for our children. Together, we can make this school year a successful and empowering experience for all students with T1D.
Preparing Your Child with T1D for a Successful School Year
Navigating the back-to-school season with a child who has T1D can be challenging, but with the right strategies and support, it can also be incredibly rewarding. By implementing these practical tips from Jen Poston, you can help your child manage their condition effectively and confidently. Open communication, thorough preparation, and fostering independence are key to ensuring your child’s success.
Remember, you are part of a larger community of parents and caregivers who understand the unique challenges of managing T1D. For more insights, check out our companion blog, “Back to School with T1D,” which offers additional strategies to create a supportive environment for your child.
Your involvement and advocacy are crucial. Supporting Diabetes Research Connection through donations can further research and provide better resources for everyone affected by T1D. Together, we can make an impact and ensure a brighter, healthier future for our children.