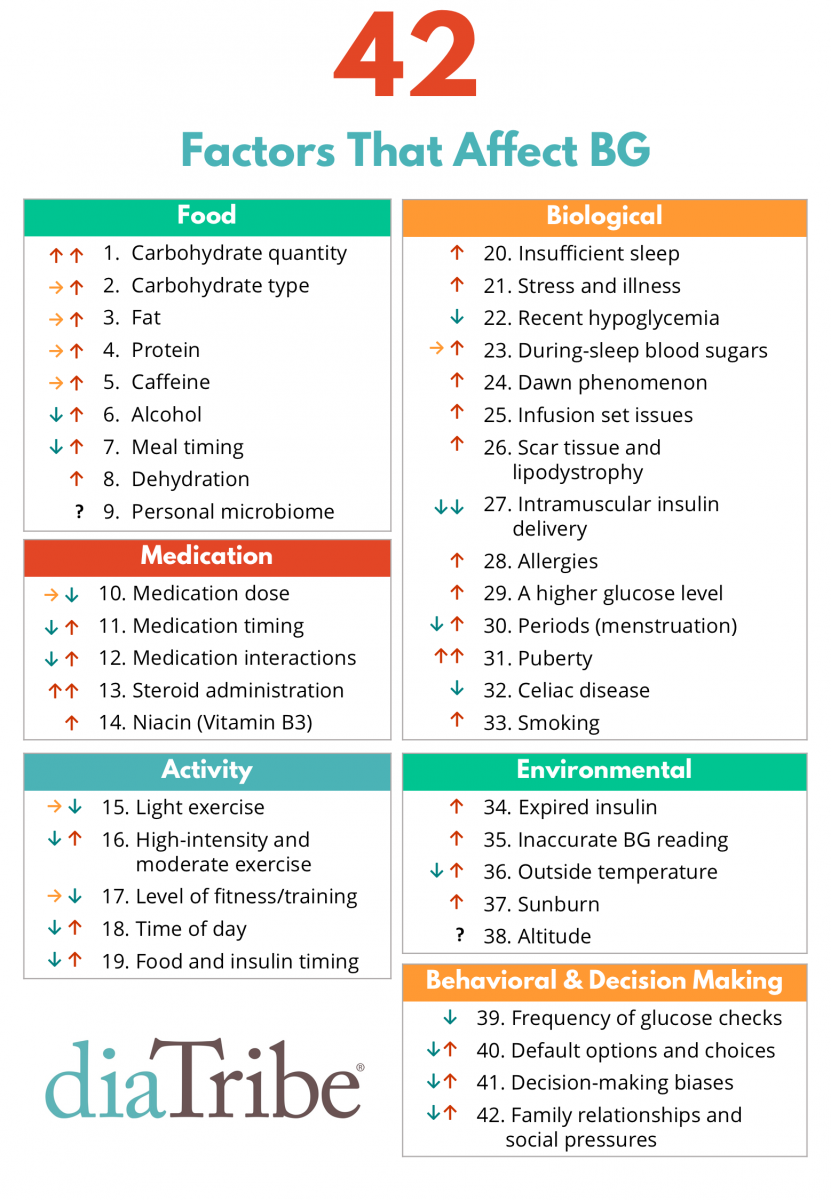
42 Factors That Affect Blood Glucose
Welcome to the Diabetes Research Connection, your trusted platform for valuable insights on diabetes management. Here we explore the above, “42 Factors That Affect BG”. Understanding these factors is crucial for anyone diagnosed with type 1 diabetes, health care providers, family and friends about how our bodies regulate blood sugar levels.
FOOD
1. Carbohydrate Quantity: Understanding carbohydrate intake is important for those with diabetes. Consider portion control and learn to read food labels. Remember, balancing carbohydrates with other food groups can help to stabilize blood sugar levels.
2. Carbohydrate Type: Opt for complex carbohydrates such as whole grains, fruits, and vegetables. These types are digested more slowly, preventing sudden blood sugar spikes.
3. Fat: Limit the amount of saturated and trans fats, which can lead to insulin resistance. Instead, choose heart-healthy unsaturated fats found in foods like avocados, nuts, and olive oil.
4. Protein: Include lean protein sources like chicken, fish, tofu, or lentils into your meals. Protein doesn’t raise blood sugar levels significantly and can help to keep you feeling satiated.
5. Caffeine: Monitor your body’s reaction to caffeine. Some people with diabetes find that caffeine causes blood sugar fluctuations. If that’s the case, reduce your caffeine intake.
6. Alcohol: If you choose to drink alcohol, do so in moderation and never on an empty stomach, as it can cause hypoglycemia. Choose low-sugar mixers to avoid blood sugar spikes.
7. Meal Timing: Regular meal and snack times can prevent blood sugar swings. Avoid skipping meals or eating late at night.
8. Dehydration: Make sure you’re drinking plenty of water throughout the day. Dehydration can negatively impact blood sugar levels.
9. Personal Microbiome: A healthy gut microbiome is believed to influence blood sugar control. Incorporate probiotic-rich foods like yogurt and fermented foods into your diet.
MEDICATION
10. Medication Dose: Always take the correct dosage of your medications as prescribed by your healthcare provider. Any changes can cause fluctuations in your blood sugar levels.
11. Medication Timing: Take your medications at the same time every day. This consistency can greatly help in managing your blood sugar levels.
12. Medication Interactions: Be aware that certain medications can interact with your diabetes medication and impact your blood sugar levels. Always inform your healthcare provider about all the medications you’re taking.
13. Steroid Administration: Steroids can cause increased blood sugar levels. If you’re prescribed a steroid, monitor your blood sugar closely and report any prolonged high readings to your healthcare provider.
14. Niacin (Vitamin B3): While niacin is important for overall health, it can raise blood sugar levels. Make sure you are getting an appropriate amount, and monitor your blood sugar if you take a supplement.
ACTIVITY
15. Light Exercise: Regular light exercise, such as walking or gentle yoga, can help control blood sugar levels. Try to be active every day, but remember to monitor your blood sugar before, during, and after exercise.
16.High Intensity & Moderate Exercise: Exercise is key in diabetes management. High-intensity workouts like HIIT can improve insulin sensitivity, while moderate activities like brisk walking help regulate glucose levels. However, monitor your blood sugar before, during, and after exercise to avoid hyperglycemia or hypoglycemia. Always consult your healthcare provider before starting a new fitness regimen.
17. Level of Fitness/Training: Your overall fitness level can impact how your body uses insulin. Regular exercise can improve insulin sensitivity and help manage blood sugar levels. However, intense training may cause short-term blood sugar spikes, so monitor your levels and adjust your food intake or insulin dosage as needed.
18. Time of Day: Blood sugar can fluctuate throughout the day. Monitoring your blood sugar levels at various times can help you understand your body’s patterns and adjust your routine accordingly.
19. Food & Insulin Timing: For those taking insulin, coordinating your meals and insulin dosage is crucial. The timing will depend on your specific needs and the type of insulin you’re using.
BIOLOGICAL
20. Too Little Sleep: Lack of sleep can disrupt your body’s insulin usage. Try to get at least 7-9 hours of sleep each night to help regulate your blood sugar.
21. Stress & Illness: Stress and illness can cause blood sugar levels to spike. Find stress management techniques that work for you, such as meditation or deep breathing exercises, and remember to monitor your blood sugar closely when you’re sick.
22. Recent Hypoglycemia: If you’ve recently experienced a bout of hypoglycemia, your body may release hormones that cause your blood sugar to rise. It’s important to monitor your blood sugar levels closely to prevent a “rebound” high.
23. During-Sleep Blood Sugars: Overnight blood sugar levels can fluctuate. Consider using a continuous glucose monitor to track your levels while you sleep.
24. Dawn Phenomenon: This is a surge in hormones that happens in the early morning, often causing an increase in blood sugar. Adjusting medication or food intake before bed can help manage this.
25. Infusion Set Issues: If you use an insulin pump, issues with the infusion set, like kinks or blockages, can affect insulin delivery and cause blood sugar fluctuations. Regularly check your infusion set to prevent issues.
26. Scar Tissue & Lipodystrophy: If you inject insulin, rotate your injection sites to avoid developing scar tissue, which can impact insulin absorption.
27. Intramuscular Insulin Delivery: Avoid injecting insulin into the muscle, as it may be absorbed too quickly, causing blood sugar fluctuations. Inject insulin into the fatty layer just beneath your skin.
28. Allergies: If you have food allergies, make sure you’re aware of how different foods affect your blood sugar levels. Also, some allergies can increase stress hormones, leading to blood sugar spikes.
29. A Higher BG Level (Glucotoxicity): High blood sugar can, in turn, cause blood sugar to rise further. Regular monitoring can help you prevent these spikes.
30. Periods (Menstruation): Hormonal fluctuations during your menstrual cycle can impact blood sugar levels. You may need to adjust your food intake or medication doses during this time.
31. Puberty: Hormonal changes during puberty can lead to increased insulin resistance. Regular monitoring and adjustment of medication doses can help manage blood sugar levels during this time.
32. Celiac Disease: If you have celiac disease, adhering to a gluten-free diet is important to avoid inflammation and nutrient malabsorption, which can impact blood sugar control.
33. Smoking: Smoking can increase insulin resistance and lead to higher blood sugar levels. Quitting smoking can significantly improve your blood sugar control.
ENVIRONMENTAL
34. Expired Insulin: Always check the expiration date on your insulin. Expired insulin is less effective and can lead to higher blood sugar levels.
35. Inaccurate BG Reading: Regularly calibrate your blood glucose meter and check strips for accuracy to ensure your readings are accurate.
36. Outside Temperature: Extreme cold or hot temperatures can impact your blood sugar levels and how your body uses insulin. Try to stay in a moderate temperature environment when possible.
37. Sunburn: Sunburn can cause stress on the body, leading to higher blood sugar levels. Protect your skin when spending time in the sun.
38. Altitude: High altitudes can impact blood sugar control. If you’re traveling to a high-altitude area, monitor your blood sugar closely and discuss any necessary medication adjustments with your healthcare provider.
BEHAVIOR & DECISIONS
39. More Frequent BG Checks: Frequent blood glucose checks can help you better understand your body’s patterns and make necessary adjustments to your diet or medication routine.
40. Default Options and Choices:
Plate/Bowl Size: The size of your plate or bowl can significantly influence portion control, a crucial factor in maintaining healthy blood sugar levels. Larger dishware tends to make us serve and consume more food than we need. By opting for smaller plates and bowls, you can naturally limit portion sizes, reducing overall carbohydrate intake and better managing your blood glucose levels.
Visual Prompts: Visual prompts play a significant role in our dietary choices. Keeping healthy food options visible and within reach encourages better food choices. Conversely, keeping high GI foods, like white bread and white rice, out of immediate sight can discourage unnecessary snacking, assisting in blood sugar control. A well-arranged fridge or pantry, with fresh fruits, vegetables, and whole grains at eye level, can serve as a constant visual prompt for healthy eating.
41. Decision-Making Biases:
Present Bias (Hyperbolic Discounting): Present bias refers to the tendency to prioritize immediate gratification over long-term benefits—a mindset that can sabotage diabetes management. For example, you might choose a sugary treat for immediate satisfaction, disregarding the long-term impact on your blood sugar levels. It’s essential to be aware of this bias and consciously make choices that favor long-term health.
Loss Aversion: This is the tendency to fear losses more than we value gains. In the context of diabetes, loss aversion might manifest as a fear of losing out on favorite foods. Shifting this mindset to focus on the gains, like improved health and energy levels when you control your blood sugar, can be a powerful motivator.
Negativity Bias: Negativity bias is the inclination to focus more on negative outcomes than positive ones. If you’ve had a bad experience with high or low blood sugar, you may become overly cautious or anxious. Remember, everyone with diabetes has good and bad days. Focus on the progress you’ve made and the tools you have to manage your condition.
Selective Matching: Selective matching involves making decisions based on memorable, though not necessarily representative, past experiences. For instance, if you had a hypoglycemic episode after a particular activity, you might avoid it completely. It’s important to remember that many factors can influence blood sugar levels, and what happened once might not happen again.
Representative Bias: Representative bias is the tendency to draw conclusions based on stereotypes or preconceptions. For example, assuming that all “sugar-free” products are good for blood glucose control can lead you astray. Always check the nutritional information, as these products can still contain other carbohydrates or unhealthy ingredients.
42. Family Relationships & Social Pressure: Communicate with your family and friends about your diabetes management needs. They can provide support and help you stick to your health goals.
In conclusion, many factors contribute to the intricate balance of blood glucose regulation. Understanding these factors aids in managing diabetes effectively and maintaining optimal health. As always, our Diabetes Research Connection team encourages everyone, especially those diagnosed with type 1 or 2 diabetes, to educate themselves about the numerous factors affecting blood glucose. It’s not just about counting carbs; it’s about comprehending the complexity of your body and the many elements that can influence your blood glucose levels.
Adam Brown, a recognized contributor at diaTribe, meticulously compiled this list of 42 factors that influence blood glucose in Type 1 Diabetes. You heard it right, not one, not two, but 42 distinct variables. In his article, Adam states “I know what you’re thinking – 42 factors that affect blood glucose? Are you kidding?!”
The answer is yes, it is indeed a formidable task, but it’s essential to see it as a testament to the daily challenges we face and overcome.
To learn more about this AMAZING list and organization, click here.