Month: July 2023
-

The Fascinating History of Diabetes
Introduction to Mellitus What’s Mellitus? Unraveling the threads of human history often reveals fascinating insights into our shared past. One such thread that has intricately woven itself into our narrative […]
-
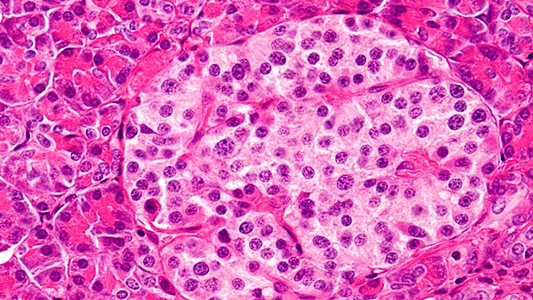
FDA Approves Lantidra – a promising cellular therapy for Type 1 Diabetes
Big Picture · On June 28, the FDA approved Lantidra, which is the first cellular therapy to treat type one diabetes. (FDA Press release) · 21 out of 30 participants […]
