Month: April 2021
-
Type 1 Diabetes May Impact Women’s Reproductive Lifespan
A woman’s reproductive stage lasts from the time of her first menstrual period (menarche) to her very last menstrual period (menopause). However, the body’s insulin production plays an integral part […]
-
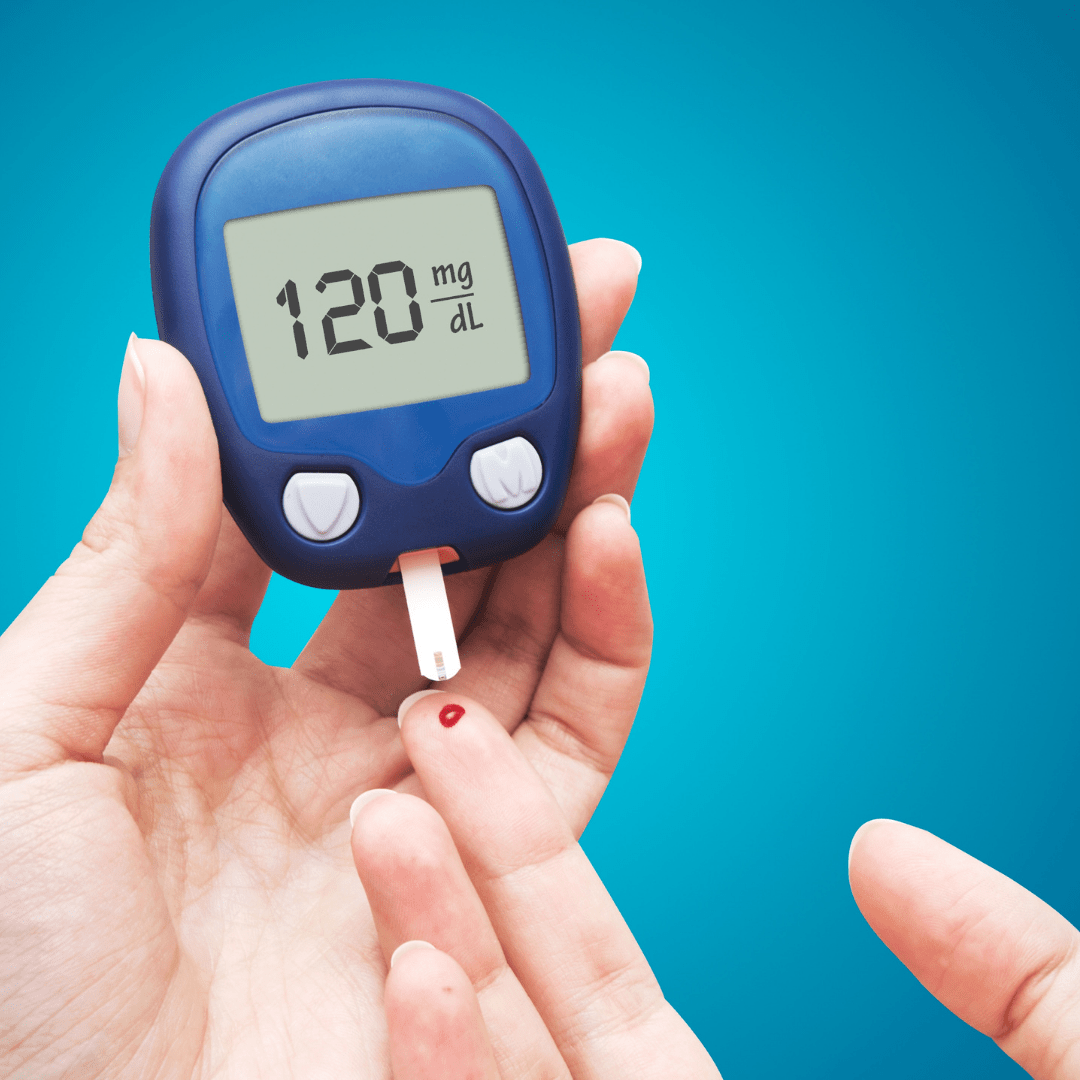
Blood Sugar Control for Type 1 Diabetes Improves During Lockdown
Type 1 diabetes is a condition that must be managed around the clock. Whether the individual is at home, work, school, practice, or out with friends, they must always be […]
-

A Push for Inpatient Use of Continuous Glucose Monitors
Many patients with type 1 diabetes (T1D) use continuous glucose monitors (CGMs) while at home to track their blood glucose levels. These devices measure the amount of glucose in the […]
-

Discussing Diabetes with DRC’s T1Ds: Blog Post 3 of Series 2
I used to hate exercising. It made my blood glucose difficult to control: one moment my levels would be rising rapidly, and then they would plummet. When I played beach […]
-

Double Trouble: A Tale of Two T1D Sisters
There are certain attributes siblings commonly share: maybe it’s a similar eye color, or smile, or a love for the same type of music. For my sister, Kyra, and me, […]
-
Feedback Superstar Shout Out!
Reach Supsterstar Status, Like Megan “Interning at DRC has been an amazing opportunity, allowing me to take my part in helping the T1D community and supporting the research being done in […]
-
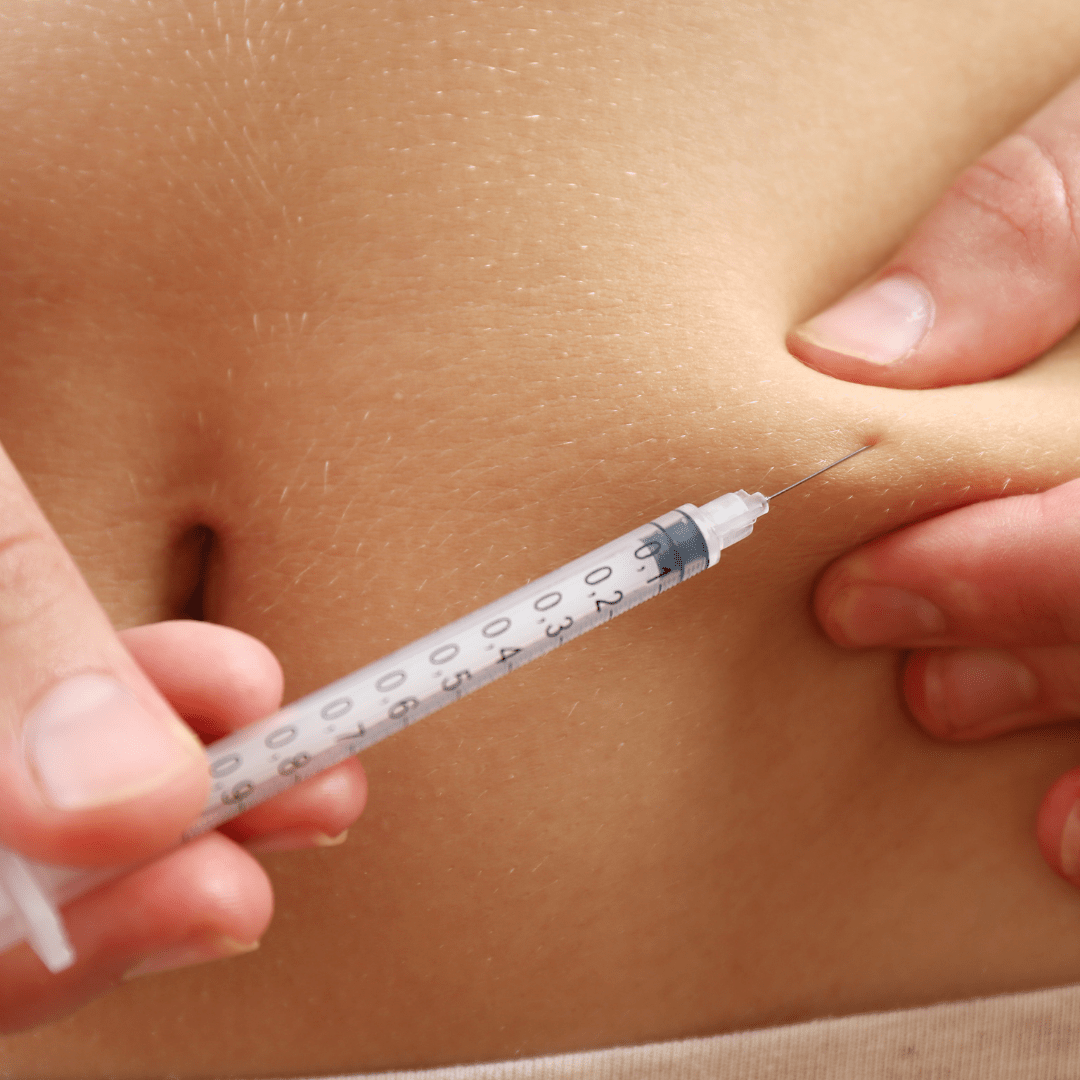
Repurposing Existing Drugs for Potential Treatment of Type 1 Diabetes
Type 1 diabetes is one of many autoimmune disorders that exist. In this particular disease, the immune system mistakenly attacks and destroys insulin-producing beta cells, leaving the body unable to […]
