Month: May 2018
-
Are Artificial Pancreas Systems Effective in Treating Type 1 Diabetes?
There are many options available for treating type 1 diabetes from regular finger pricks and injections of insulin to continuous glucose monitoring systems to artificial pancreases and more. However, each […]
-
Viruses May Cause T1D and Other Autoimmune Diseases
Viruses are the cause of many health conditions and affect the body in different ways. As scientists learn more about these viruses, they can develop targeted strategies for preventing and […]
-
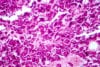
Oxygen Supply May be Key in Supporting Islet Transplantation
One of the strategies scientists have focused on in the treatment of type 1 diabetes is transplanting healthy islet cells into the body to naturally produce insulin and manage blood […]