Month: October 2017
-

Gallbladder Cells May Be A Viable Source for Treating Type 1 Diabetes
One of the main focuses of many studies regarding type 1 diabetes is how to generate new cells or reprogram existing cells to function as insulin-producing beta cells. Scientists have […]
-
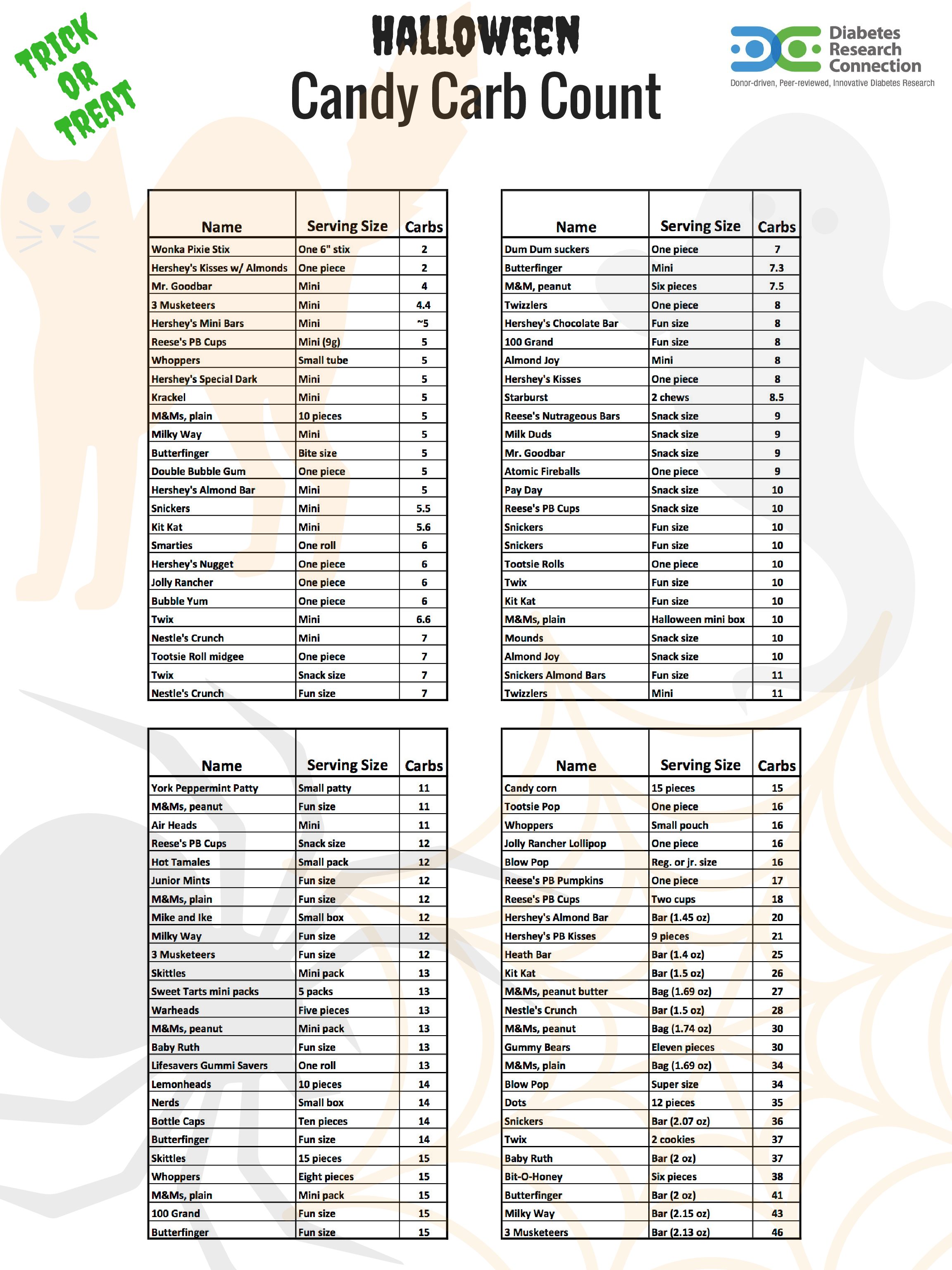
Halloween Candy Carbohydrate Counts for People with T1D
Understanding T1D Carbohydrate counts are important with people with diabetes. The spookiest part of Halloween for people with Type 1 Diabetes (T1D) isn’t ghosts or ghouls; it’s the carb-loaded candies. […]
-

Simpler Measuring Technique May Help Identify Partial Clinical Remission in Type 1 Diabetes
One of the major challenges of type 1 diabetes is effectively managing blood glucose levels. It is a careful balancing act and differs for every patient. With type 1 diabetes, […]
-
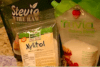
HOW TO MAKE RECIPES MORE DIABETIC FRIENDLY
One of the things that we’ll do more of in the future for Sweet Talkers is to discuss how to lower the number of carbohydrates in a recipe. For example, […]
-
What Gene Editing Could Mean for Type 1 Diabetes
Altering human genetics is a sensitive subject. There are a lot of things that could potentially go wrong, but also many that could go right. CRISPR/Cas9 technology allows scientists to […]
-
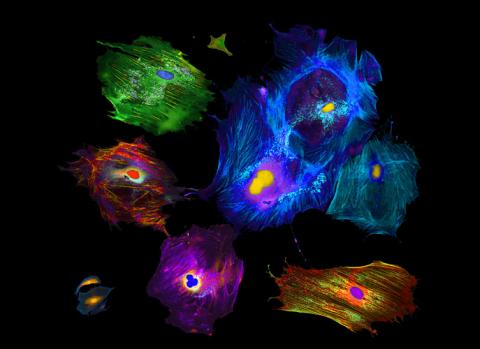
Tackling Type 1 Diabetes at a Cellular Level
In individuals with type 1 diabetes, the body mistakenly attacks insulin-producing cells and destroys them. This leaves the body unable to regulate the amount of sugar in the blood or […]
-

Could Beta Cell Age and Differentiation Play a Role in the Development of Diabetes?
The exact cause of type 1 diabetes is yet unknown. Researchers have a good understanding of how type 1 diabetes works and impacts the body, but not of the cellular […]
