Month: December 2016
-
New Weapon Against Diabetes
Original article published by ETH Zurich on December 1, 2016. Click here to read the original article. Researchers have used the simplest approach yet to produce artificial beta cells from human […]
-
Meet the DRC Board: Alberto Hayek, M.D.
At the Diabetes Research Connection, our passion is working together with the scientific community to find a way to treat, cure and prevent type 1 diabetes, and our board is […]
-

Economic 3D-Printing Approach for Transplantation of Human Stem Cell-Derived β-Like Cells
Original article published by IOP Science on December 1, 2016. Click here to read the original article. Abstract Transplantation of human pluripotent stem cells (hPSC) differentiated into insulin-producing βcells is a […]
-

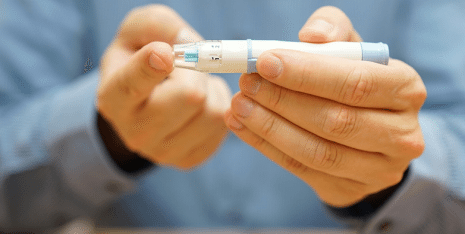
Holiday Travel Tips for Those With T1D
The holiday season is in full swing, and many of us will be traveling this month to visit friends, family and loved ones. For those with type 1 diabetes (T1D), […]
-

“Artificial Pancreas” Is Approved
Original article published by The JAMA Network on October 4, 2016. Click here to read the original article. A new device that automatically monitors blood glucose levels and adjusts insulin levels […]
