Month: January 2016
-
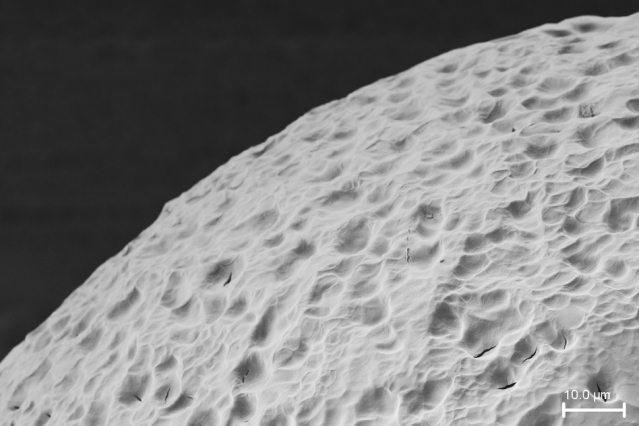
No More Insulin Injections?
Original article written by Anne Trafton for MIT News Office on January 26, 2016. Click here to read the original article. In patients suffering from Type 1 diabetes, the immune system […]
-
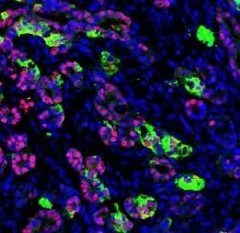
Insulin-Producing Pancreatic Cells Created from Human Skin Cells
Original article written by Dana Smith for Gladstone Institutes on January 6, 2016. Click here to read the original article. SAN FRANCISCO, CA—Scientists at the Gladstone Institutes and the University of […]
