Month: August 2015
-

Prolonged Antibiotic Treatment Induces A Diabetogenic Intestinal Microbiome That Accelerates Diabetes In NOD Mice
Accumulating evidence supports that the intestinal microbiome is involved in Type 1 diabetes (T1D) pathogenesis through the gut-pancreas nexus.
-
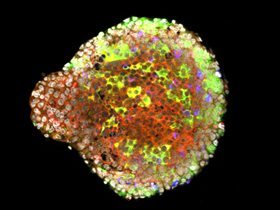
Bacteria That Prevents Type 1 Diabetes
Our bodies have ten times the amount of microbes than human cells. This set of bacteria is called microbiota. In some instances, bacteria known as pathogens can cause infectious diseases.
-

How Can YOU Influence the Future of Type 1 Diabetes Research?
Novel crowdfunding platform connecting donors directly with early-career scientists, enabling them to perform peer-reviewed, innovative research in type 1 diabetes.
