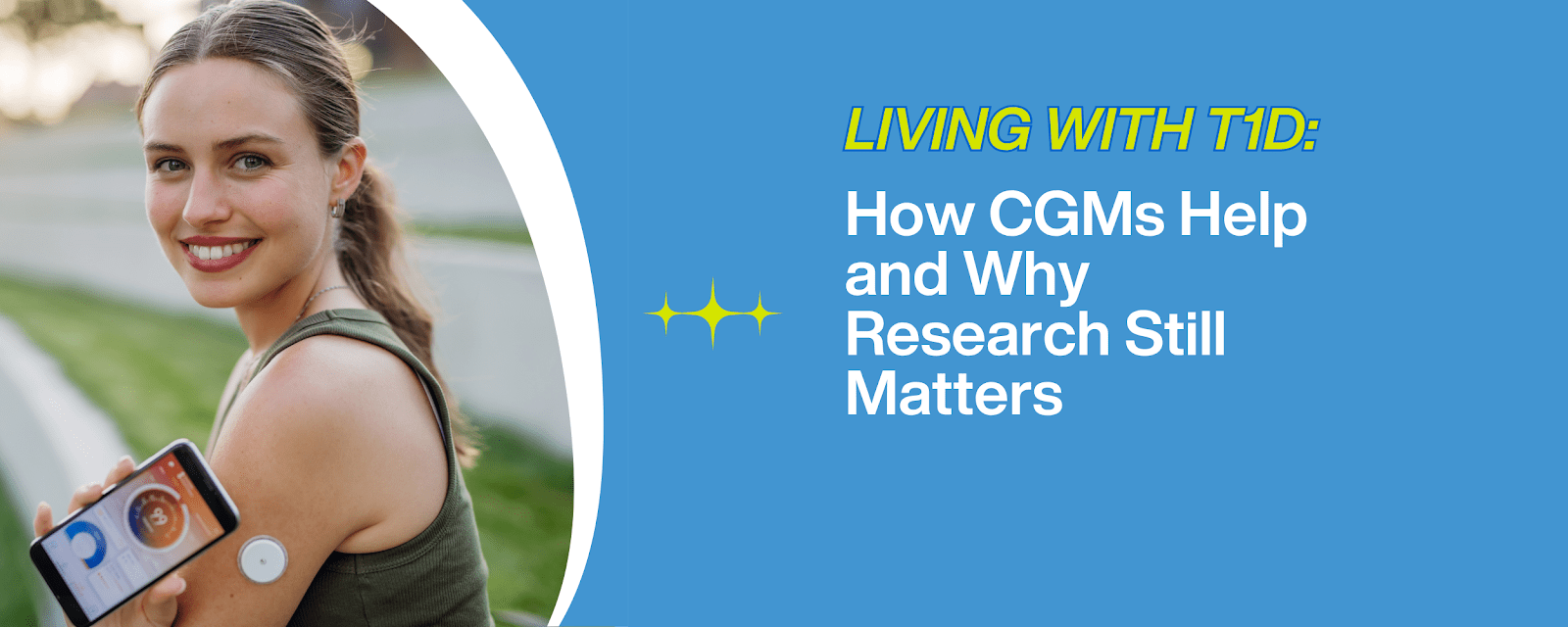
For people living with type 1 diabetes (T1D), managing blood sugar isn’t just a daily task—it’s a 24/7 responsibility. Thankfully, Continuous Glucose Monitors (CGMs) have transformed the way this condition is managed.
But how much of a difference do these tools make? And what challenges remain?
To find out, we spoke with Brooklynn Hamilton, Development Director at Diabetes Research Connection (DRC) and someone who lives with T1D.
“Technological advancements have transformed survival into management, granting me a greater sense of independence and safety,” says Brooklynn. “Yet, they do not eliminate the reality of living with this disease. My body is constantly in conversation with machines, numbers, and alerts – .so while they have brought me convenience, they haven’t brought peace.”
Her words capture a key truth for many in the T1D community: while technology helps, it doesn’t erase the burden.
What Is a CGM?
A Continuous Glucose Monitor is a small, wearable device that automatically tracks glucose levels around the clock, reducing the need for frequent finger pricks.
Key Components:
- Sensor: Inserted under the skin, usually on the arm or abdomen
- Transmitter: Sends data wirelessly
- Receiver or App: Displays real-time glucose data and trends
How Does Continuous Glucose Monitoring Work?
Unlike fingerstick tests that offer a single snapshot reading, CGMs track trends and warn users about dangerous highs or lows.
Top Benefits:
- Real-time alerts for highs and lows
- Fewer finger pricks
- Better insights into on how food, stress, and exercise affect blood sugar
- Peace of mind for users and loved ones
- Easy data sharing with healthcare teams
Brooklynn agrees these tools have enhanced her independence and safety. Still, they require attention and effort:
“High-tech solutions do not equate to low maintenance; I still closely monitor my devices and make crucial daily decisions that significantly impact my health. Both technology and my body can be unpredictable, so I must trust my instincts and stay vigilant 24/7.”
Who Uses a CGM?
Originally for people with T1D, CGMs are now also used by:
- Individuals with insulin-dependent type 2 diabetes
- Those with frequent glucose fluctuations and type 1 diabetes risk factors
Many insurance plans cover them, and modern CGMs are smaller, more comfortable, and last up to 14 days.
Is It Painful?
Most users describe the sensor insertion as a brief pinch. Once applied, the device becomes almost unnoticeable until it needs replacement.
Do You Still Need Fingersticks?
Some models, like Dexcom G6 and G7, require no calibration. Others may still need occasional checks for accuracy.
Choosing the Right CGM
Popular options include:
- Dexcom G6/G7: Real-time alerts, strong mobile integration
- FreeStyle Libre 2/3: Affordable, easy to apply, scan-to-read
- Medtronic Guardian Connect: Works with compatible insulin pumps
When looking for the best CGM for type 1 diabetes, consider these factors:
- How long the sensor lasts
- Smartphone or pump compatibility
- Alert features
- Cost and insurance coverage
So, What’s Next?
While CGM technology makes diabetes more manageable, users like Brooklynn remind us that it’s not a cure.
“Innovation buys us time, but a cure will grant us our freedom,” says Brooklynn. “I am alive because of visionaries who invested in bold ideas. I hope future generations can say they are free because we invested in finding a cure.”
This is why DRC funds type 1 diabetes research studies—to improve current tools and fuel bold ideas that could one day end T1D altogether.
Support the Future of T1D Innovation
Want to help accelerate new treatments for type 1 diabetes and the search for a cure?
- Subscribe to the DRC newsletter
- Share this blog with friends and family
- Donate to support groundbreaking Type 1 Diabetes research
Together, we can turn progress into possibility—and hope into reality.